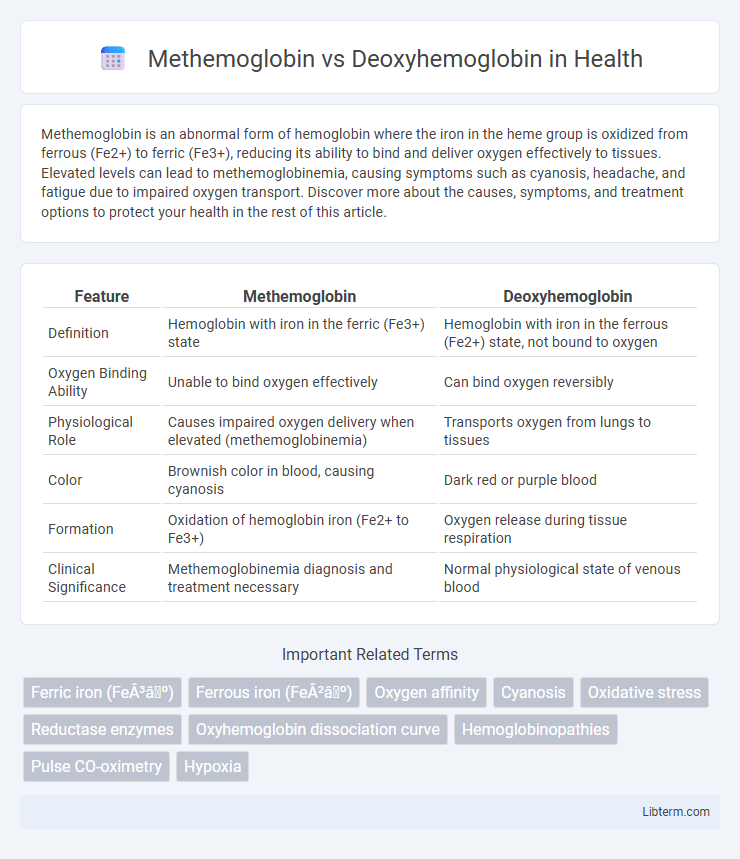
Methemoglobin is an abnormal form of hemoglobin where the iron in the heme group is oxidized from ferrous (Fe2+) to ferric (Fe3+), reducing its ability to bind and deliver oxygen effectively to tissues. Elevated levels can lead to methemoglobinemia, causing symptoms such as cyanosis, headache, and fatigue due to impaired oxygen transport. Discover more about the causes, symptoms, and treatment options to protect your health in the rest of this article.
Table of Comparison
| Feature | Methemoglobin | Deoxyhemoglobin |
|---|---|---|
| Definition | Hemoglobin with iron in the ferric (Fe3+) state | Hemoglobin with iron in the ferrous (Fe2+) state, not bound to oxygen |
| Oxygen Binding Ability | Unable to bind oxygen effectively | Can bind oxygen reversibly |
| Physiological Role | Causes impaired oxygen delivery when elevated (methemoglobinemia) | Transports oxygen from lungs to tissues |
| Color | Brownish color in blood, causing cyanosis | Dark red or purple blood |
| Formation | Oxidation of hemoglobin iron (Fe2+ to Fe3+) | Oxygen release during tissue respiration |
| Clinical Significance | Methemoglobinemia diagnosis and treatment necessary | Normal physiological state of venous blood |
Introduction to Hemoglobin Variants
Methemoglobin and deoxyhemoglobin are distinct hemoglobin variants with crucial differences in oxygen transport and biochemical properties. Methemoglobin contains iron in the ferric (Fe3+) state, preventing oxygen binding and leading to decreased oxygen delivery to tissues, whereas deoxyhemoglobin contains iron in the ferrous (Fe2+) state, allowing reversible oxygen binding essential for oxygen transport. Understanding the structural and functional disparities between these hemoglobin forms is vital for diagnosing and managing conditions like methemoglobinemia and tissue hypoxia.
What is Methemoglobin?
Methemoglobin is a form of hemoglobin in which the iron in the heme group is oxidized from the ferrous (Fe2+) to the ferric (Fe3+) state, impairing its ability to bind and transport oxygen effectively. Unlike deoxyhemoglobin, which contains iron in the ferrous state and can readily bind oxygen, methemoglobin cannot carry oxygen to tissues, leading to reduced oxygen delivery and potential hypoxia. Elevated levels of methemoglobin, known as methemoglobinemia, result from oxidative stress or exposure to certain drugs and chemicals, requiring medical intervention to restore normal hemoglobin function.
What is Deoxyhemoglobin?
Deoxyhemoglobin is the form of hemoglobin that lacks bound oxygen, found primarily in venous blood where oxygen has been released to tissues. It differs from methemoglobin, which contains oxidized iron (Fe3+) and cannot bind oxygen effectively, impairing oxygen transport. The reversible binding of oxygen to deoxyhemoglobin is essential for maintaining tissue oxygenation and normal respiratory function.
Structural Differences Between Methemoglobin and Deoxyhemoglobin
Methemoglobin contains iron in the ferric (Fe3+) state, which prevents it from binding oxygen, while deoxyhemoglobin contains iron in the ferrous (Fe2+) state capable of oxygen binding. Structurally, methemoglobin exhibits a distorted heme environment due to the oxidation of iron, leading to altered protein conformation and reduced oxygen affinity. Deoxyhemoglobin maintains a planar heme group with iron positioned slightly out of the plane, facilitating reversible oxygen binding critical for oxygen transport.
Oxygen Binding Affinity Comparison
Methemoglobin contains iron in the ferric (Fe3+) state, which prevents it from effectively binding oxygen, leading to significantly reduced oxygen affinity compared to deoxyhemoglobin, where the iron is in the ferrous (Fe2+) state. Deoxyhemoglobin readily binds oxygen in the lungs, transitioning to oxyhemoglobin, whereas methemoglobin cannot participate in oxygen transport, thereby impairing oxygen delivery to tissues. The elevated presence of methemoglobin in blood conditions, known as methemoglobinemia, results in decreased overall oxygen-binding capacity and diminished tissue oxygenation.
Causes and Formation Mechanisms
Methemoglobin forms when the iron in hemoglobin is oxidized from the ferrous (Fe2+) to the ferric (Fe3+) state, impairing its ability to bind oxygen; this oxidation can result from exposure to certain drugs, chemicals, or genetic defects affecting methemoglobin reductase. Deoxyhemoglobin arises when oxygen dissociates from oxyhemoglobin during normal tissue respiration, returning hemoglobin to its reduced ferrous state without oxygen binding. While methemoglobin accumulates due to oxidative stress and enzymatic deficiencies, deoxyhemoglobin represents the physiologically normal form of hemoglobin during oxygen delivery to tissues.
Physiological Roles and Significance
Methemoglobin contains oxidized iron (Fe3+) that cannot bind oxygen, playing a minimal physiological role but serving as an indicator of oxidative stress and certain toxic exposures. Deoxyhemoglobin, with iron in the reduced Fe2+ state, is critical for oxygen release in tissues and maintaining oxygen delivery under varying physiological conditions. The balance between methemoglobin and deoxyhemoglobin levels reflects the body's oxygen transport efficiency and redox state, impacting tissue oxygenation and cellular metabolism.
Clinical Implications and Disorders
Methemoglobin, characterized by the oxidation of the heme iron to the ferric (Fe3+) state, impairs oxygen delivery and leads to methemoglobinemia, which presents clinically with cyanosis and hypoxia despite normal oxygen partial pressure. Deoxyhemoglobin, the reduced form of hemoglobin without bound oxygen, is pivotal in tissue oxygen release but elevated levels in venous blood can indicate impaired oxygenation or circulatory issues. Understanding the distinction between methemoglobinemia and conditions involving abnormal deoxyhemoglobin concentrations informs diagnosis and treatment strategies for hypoxic disorders and hemoglobinopathies.
Diagnostic Methods and Detection
Methemoglobin and deoxyhemoglobin are distinguished through specific diagnostic methods using co-oximetry, which measures absorbance at multiple wavelengths to accurately quantify different hemoglobin species. Pulse CO-oximeters provide non-invasive detection of methemoglobin levels, aiding rapid diagnosis in suspected methemoglobinemia cases. Spectrophotometric analysis remains a gold standard for laboratory detection, delivering precise differentiation between methemoglobin and deoxyhemoglobin in blood samples.
Treatment and Management Strategies
Treatment of methemoglobinemia primarily involves the administration of methylene blue, which acts as a reducing agent to convert methemoglobin back to functional hemoglobin. In contrast, deoxyhemoglobin management focuses on improving oxygen delivery through supplemental oxygen therapy and addressing underlying causes such as respiratory or cardiovascular conditions. Severe cases of methemoglobinemia may require exchange transfusion or hyperbaric oxygen therapy, whereas deoxyhemoglobin-related hypoxia necessitates targeted interventions to restore adequate tissue oxygenation.
Methemoglobin Infographic
 libterm.com
libterm.com