Proteinuria indicates the presence of excess protein in the urine, often signaling kidney damage or disease. Early detection and management are crucial to prevent complications such as chronic kidney disease or cardiovascular issues. Learn more about the causes, symptoms, and treatments of proteinuria in the rest of the article.
Table of Comparison
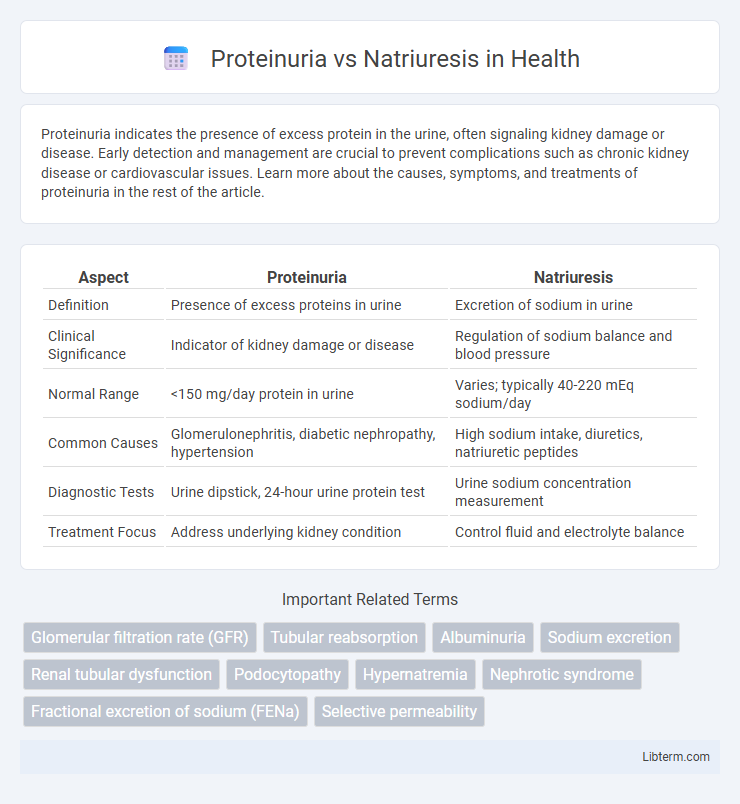
| Aspect | Proteinuria | Natriuresis |
|---|---|---|
| Definition | Presence of excess proteins in urine | Excretion of sodium in urine |
| Clinical Significance | Indicator of kidney damage or disease | Regulation of sodium balance and blood pressure |
| Normal Range | <150 mg/day protein in urine | Varies; typically 40-220 mEq sodium/day |
| Common Causes | Glomerulonephritis, diabetic nephropathy, hypertension | High sodium intake, diuretics, natriuretic peptides |
| Diagnostic Tests | Urine dipstick, 24-hour urine protein test | Urine sodium concentration measurement |
| Treatment Focus | Address underlying kidney condition | Control fluid and electrolyte balance |
Overview of Proteinuria and Natriuresis
Proteinuria is characterized by an abnormal amount of protein, primarily albumin, in the urine, often indicating kidney damage or disease such as glomerulonephritis or diabetic nephropathy. Natriuresis refers to the excretion of sodium in the urine, a process regulated by hormonal factors including aldosterone and natriuretic peptides, playing a critical role in blood pressure and fluid balance. Both proteinuria and natriuresis serve as important clinical biomarkers for diagnosing and managing renal and cardiovascular conditions.
Definitions: Proteinuria vs Natriuresis
Proteinuria refers to the presence of an abnormal amount of protein in the urine, often indicating kidney damage or disease affecting the glomerular filtration barrier. Natriuresis is the process of sodium excretion in the urine, regulated by renal mechanisms to maintain sodium balance and blood pressure homeostasis. While proteinuria signals impaired kidney function, natriuresis reflects the kidney's role in electrolyte and fluid regulation.
Underlying Mechanisms and Causes
Proteinuria results from glomerular damage or increased permeability of the kidney's filtration barrier, allowing proteins like albumin to leak into the urine, commonly caused by conditions such as diabetes mellitus, hypertension, and glomerulonephritis. Natriuresis involves increased sodium excretion primarily due to alterations in renal tubular sodium handling, influenced by factors like high salt intake, volume expansion, and hormones such as atrial natriuretic peptide (ANP) and aldosterone. While proteinuria reflects structural or functional glomerular pathology, natriuresis is predominantly a regulatory response of the distal nephron maintaining sodium balance and blood pressure.
Clinical Significance and Implications
Proteinuria indicates abnormal kidney filtration due to glomerular damage, signaling conditions like chronic kidney disease or diabetic nephropathy and increasing the risk of cardiovascular complications. Natriuresis reflects renal sodium excretion influenced by volume status and neurohormonal regulation, playing a critical role in managing hypertension and heart failure by affecting fluid balance. Both markers guide clinical decisions on diagnosing, monitoring, and treating renal and cardiovascular disorders through targeted interventions.
Diagnostic Methods: Proteinuria
Proteinuria diagnosis primarily involves the quantitative measurement of albumin or total protein in urine using spot urine albumin-to-creatinine ratio (ACR) or 24-hour urine protein collection tests. Diagnostic accuracy increases with immunoassays such as immunonephelometry or immunoturbidimetry, which differentiate albumin from other proteins. Automated dipstick tests provide rapid screening but require confirmation by more specific laboratory methods to assess kidney function and severity of protein loss.
Diagnostic Methods: Natriuresis
Natriuresis is primarily assessed through 24-hour urine sodium excretion measurements, which provide quantitative data on kidney sodium handling and aid in diagnosing conditions such as hyponatremia or volume status abnormalities. Spot urine sodium tests combined with urine creatinine can estimate natriuresis efficiently when 24-hour collection is impractical. Advanced diagnostic imaging and blood tests are typically reserved for investigating underlying causes affecting natriuresis, including adrenal or renal disorders.
Common Conditions Associated with Proteinuria
Proteinuria is commonly associated with kidney diseases such as diabetic nephropathy, glomerulonephritis, and hypertensive nephrosclerosis, reflecting damage to the glomerular filtration barrier. Unlike natriuresis, which primarily involves sodium excretion often triggered by volume expansion or diuretic use, proteinuria directly indicates abnormal protein leakage due to renal pathology. Monitoring proteinuria levels is crucial for diagnosing and managing chronic kidney disease, as persistent proteinuria correlates with disease progression and cardiovascular risk.
Common Conditions Associated with Natriuresis
Natriuresis, the excretion of sodium in the urine, is commonly associated with conditions such as congestive heart failure, cirrhosis, and nephrotic syndrome, where altered sodium balance contributes to fluid retention and edema. In contrast, proteinuria, the presence of excess protein in the urine, typically indicates glomerular damage linked to diseases like diabetic nephropathy and glomerulonephritis. Monitoring natriuresis helps assess effective sodium handling in volume overload states, while proteinuria is a key marker for kidney injury and disease progression.
Treatment Approaches and Management Strategies
Treatment approaches for proteinuria primarily involve controlling underlying conditions such as diabetes and hypertension using ACE inhibitors or ARBs to reduce protein excretion and protect kidney function. Management strategies for natriuresis focus on addressing the underlying causes like heart failure or liver cirrhosis, often through diuretics to promote sodium excretion and fluid balance regulation. Both conditions require careful monitoring of electrolytes and renal function to optimize therapeutic efficacy and prevent complications.
Key Differences and Clinical Considerations
Proteinuria refers to the abnormal presence of protein in the urine, indicating kidney damage or disease, while natriuresis involves the excretion of sodium in the urine, reflecting fluid and electrolyte balance. Clinically, proteinuria is often assessed to diagnose and monitor renal conditions like glomerulonephritis or diabetic nephropathy, whereas natriuresis is evaluated in cases of hypertension, heart failure, or volume overload. Understanding these processes aids in targeted treatment strategies, such as managing proteinuria with renin-angiotensin system inhibitors and addressing natriuresis through diuretics or sodium intake regulation.
Proteinuria Infographic
 libterm.com
libterm.com