Cholecystitis occurs when the gallbladder becomes inflamed, often due to gallstones blocking the bile ducts, leading to severe abdominal pain, fever, and digestive issues. Cholelithiasis refers to the presence of gallstones within the gallbladder, which may remain asymptomatic or cause discomfort and complications if left untreated. Understanding the differences, symptoms, and treatment options is essential for managing your gallbladder health--read on to learn more.
Table of Comparison
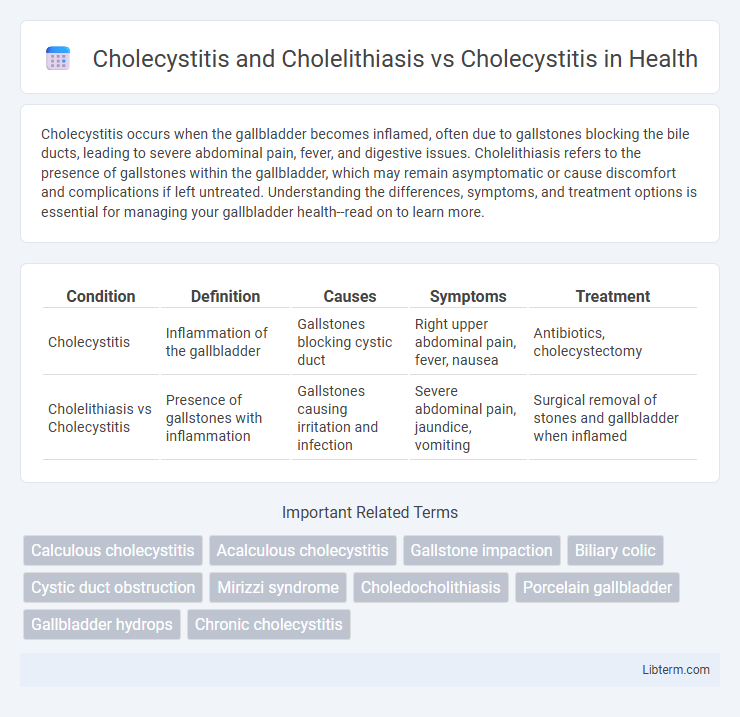
| Condition | Definition | Causes | Symptoms | Treatment |
|---|---|---|---|---|
| Cholecystitis | Inflammation of the gallbladder | Gallstones blocking cystic duct | Right upper abdominal pain, fever, nausea | Antibiotics, cholecystectomy |
| Cholelithiasis vs Cholecystitis | Presence of gallstones with inflammation | Gallstones causing irritation and infection | Severe abdominal pain, jaundice, vomiting | Surgical removal of stones and gallbladder when inflamed |
Overview of Cholecystitis and Cholelithiasis
Cholecystitis is the inflammation of the gallbladder, commonly caused by gallstones obstructing the cystic duct, a condition known as cholelithiasis. Cholelithiasis refers specifically to the presence of gallstones, which can lead to complications like acute or chronic cholecystitis if not addressed. Understanding the distinction highlights that cholelithiasis is a primary risk factor and underlying cause of many cholecystitis cases, emphasizing the importance of diagnosing gallstones to prevent gallbladder inflammation.
Pathophysiology: Gallstones and Gallbladder Inflammation
Cholecystitis and cholelithiasis often coexist, where gallstones (cholelithiasis) obstruct the cystic duct, leading to gallbladder inflammation (cholecystitis) due to bile stasis and bacterial infection. Inflammation results from mechanical irritation and secondary infection, causing mucosal damage, edema, and ischemia of the gallbladder wall. Cholecystitis without gallstones (acalculous cholecystitis) arises from gallbladder hypomotility, ischemia, or infection without obstruction, highlighting the distinct yet overlapping pathophysiology of gallbladder diseases.
Types of Cholecystitis: Calculous vs. Acalculous
Cholecystitis primarily manifests as calculous or acalculous types, with calculous cholecystitis caused by gallstones obstructing the cystic duct, accounting for approximately 90-95% of cases. Acalculous cholecystitis, representing 5-10% of cases, occurs without gallstones, often linked to critical illness, trauma, or prolonged fasting, and presents a higher risk of complications. The presence or absence of cholelithiasis (gallstones) significantly influences clinical management, prognosis, and treatment strategies for cholecystitis patients.
Cholecystitis with Gallstones: Clinical Features
Cholecystitis with gallstones, also known as calculous cholecystitis, presents with intense right upper quadrant pain, fever, and leukocytosis due to inflammation caused by gallstone obstruction of the cystic duct. Clinical features often include Murphy's sign, nausea, vomiting, and elevated liver enzymes, reflecting biliary tract involvement. Ultrasound imaging typically reveals gallstones, gallbladder wall thickening, and pericholecystic fluid, aiding in distinguishing calculous cholecystitis from acalculous cholecystitis and isolated cholelithiasis.
Cholecystitis without Gallstones: Distinct Characteristics
Cholecystitis without gallstones, also known as acalculous cholecystitis, presents distinct clinical features from cholecystitis caused by cholelithiasis, including inflammation of the gallbladder in the absence of gallstones. This condition often occurs in critically ill patients and is associated with biliary stasis, ischemia, and infection rather than mechanical obstruction. Diagnosis relies on imaging modalities such as ultrasound or HIDA scan, with treatment strategies emphasizing antibiotics and supportive care over surgical intervention commonly required for stone-related cholecystitis.
Diagnostic Criteria: Differentiating Both Conditions
Cholecystitis diagnosis involves identifying inflammation of the gallbladder, often confirmed by ultrasound showing gallbladder wall thickening, pericholecystic fluid, and a positive Murphy's sign, whereas cholelithiasis is primarily diagnosed by detecting gallstones within the gallbladder without inflammation. Laboratory values in cholecystitis typically reveal elevated white blood cell count and increased inflammatory markers, while cholelithiasis often lacks significant systemic inflammatory response. Differentiation hinges on imaging studies combined with clinical presentation, where cholecystitis presents with acute pain and systemic signs, and cholelithiasis may be asymptomatic or cause biliary colic without inflammation.
Imaging Findings: Ultrasonography and Beyond
Cholecystitis and cholelithiasis frequently present with similar ultrasonographic features such as gallstones, gallbladder wall thickening exceeding 3 mm, and pericholecystic fluid, whereas uncomplicated cholecystitis may show gallbladder distension without stones. Advanced imaging modalities like hepatobiliary iminodiacetic acid (HIDA) scanning demonstrate cystic duct obstruction with non-visualization of the gallbladder in acute cholecystitis, whereas magnetic resonance cholangiopancreatography (MRCP) precisely delineates bile duct anatomy and detects choledocholithiasis. Contrast-enhanced computed tomography (CT) may reveal gallbladder wall enhancement and complications like emphysematous cholecystitis, providing comprehensive evaluation beyond ultrasonography.
Treatment Approaches: Medical and Surgical Options
Treatment approaches for cholecystitis and cholelithiasis primarily involve pain management, antibiotics, and surgical interventions such as laparoscopic cholecystectomy, especially in acute cases or when gallstones cause persistent symptoms. Medical management may include ursodeoxycholic acid to dissolve cholesterol gallstones in non-surgical candidates, while surgical options remain the definitive treatment to prevent recurrence and complications. Timely intervention with cholecystectomy reduces the risk of complications like gallbladder perforation or chronic cholecystitis, improving patient outcomes.
Complications: Risks of Combined vs. Isolated Cholecystitis
Cholecystitis combined with cholelithiasis significantly increases the risk of gallbladder perforation, empyema, and sepsis compared to isolated cholecystitis, which typically presents with localized inflammation. The presence of gallstones in cholelithiasis obstructs the cystic duct, exacerbating bile stasis and infection, thereby elevating the likelihood of chronic cholecystitis and gallbladder gangrene. Isolated cholecystitis, often acalculous, carries a lower risk of severe complications but may still progress to necrosis or abscess formation if untreated.
Prognosis and Prevention Strategies
Cholecystitis combined with cholelithiasis typically presents with higher risks of recurrent inflammation and gallbladder complications compared to uncomplicated cholecystitis, influencing a more guarded prognosis. Preventive strategies for cholelithiasis include dietary modification to reduce cholesterol and fat intake, weight management, and regular physical activity, which in turn lowers the incidence of cholecystitis. Timely diagnosis and cholecystectomy remain critical in preventing progression to severe complications such as gallbladder perforation or chronic cholecystitis.
Cholecystitis and Cholelithiasis Infographic
 libterm.com
libterm.com