Intrathecal administration involves delivering medication directly into the spinal canal, allowing drugs to bypass the blood-brain barrier for targeted treatment of neurological conditions. This method is commonly used for pain management, chemotherapy, and anesthesia with enhanced efficacy and fewer systemic side effects. Explore the article to understand how intrathecal therapy could optimize your treatment options.
Table of Comparison
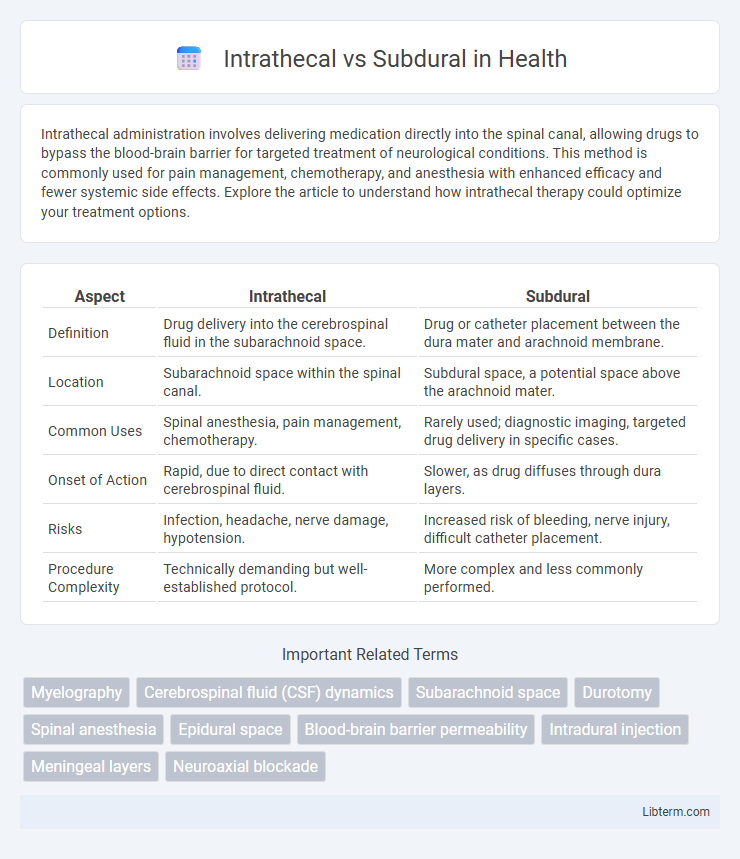
| Aspect | Intrathecal | Subdural |
|---|---|---|
| Definition | Drug delivery into the cerebrospinal fluid in the subarachnoid space. | Drug or catheter placement between the dura mater and arachnoid membrane. |
| Location | Subarachnoid space within the spinal canal. | Subdural space, a potential space above the arachnoid mater. |
| Common Uses | Spinal anesthesia, pain management, chemotherapy. | Rarely used; diagnostic imaging, targeted drug delivery in specific cases. |
| Onset of Action | Rapid, due to direct contact with cerebrospinal fluid. | Slower, as drug diffuses through dura layers. |
| Risks | Infection, headache, nerve damage, hypotension. | Increased risk of bleeding, nerve injury, difficult catheter placement. |
| Procedure Complexity | Technically demanding but well-established protocol. | More complex and less commonly performed. |
Introduction to Intrathecal and Subdural Spaces
The intrathecal space, located between the arachnoid mater and pia mater, contains cerebrospinal fluid (CSF) and serves as a critical site for administering spinal anesthesia or medications directly into the CSF. The subdural space, found between the dura mater and arachnoid mater, is a potential space that typically contains a thin layer of fluid but can expand in pathological conditions such as subdural hematomas. Understanding the anatomical differences between the intrathecal and subdural spaces is essential for safe and effective clinical procedures involving spinal and neurovascular interventions.
Anatomy: Intrathecal vs Subdural Regions
The intrathecal space, located between the arachnoid mater and the pia mater, contains cerebrospinal fluid (CSF) and houses nerve roots, making it a critical site for drug delivery in spinal anesthesia and pain management. In contrast, the subdural space is a potential space between the dura mater and arachnoid mater, usually minimal in volume and less accessible, often becoming apparent only during pathological conditions like subdural hematomas. Understanding the distinct anatomical boundaries and physiological characteristics of intrathecal versus subdural regions is essential for accurate diagnosis, effective targeted therapies, and avoiding complications in neurosurgical and anesthetic procedures.
Indications for Intrathecal and Subdural Procedures
Intrathecal procedures are primarily indicated for administering medications directly into the cerebrospinal fluid to treat chronic pain, spasticity, or central nervous system infections, ensuring rapid and targeted drug delivery. Subdural procedures are typically performed to manage subdural hematomas, relieve increased intracranial pressure, and address certain types of brain injuries or infections located between the dura mater and arachnoid mater. Choosing between intrathecal and subdural approaches depends on the specific pathology, location of the pathology, and desired therapeutic outcome within the central nervous system.
Procedure Techniques: Intrathecal vs Subdural
Intrathecal procedures involve injecting medication directly into the cerebrospinal fluid within the subarachnoid space, allowing rapid and effective delivery to the central nervous system. Subdural techniques place agents between the dura mater and arachnoid mater, resulting in a slower diffusion and typically lower drug concentration in the cerebrospinal fluid. The precision of needle placement and knowledge of spinal anatomy are critical in both methods to avoid complications such as nerve damage or infection.
Common Medications for Intrathecal and Subdural Administration
Common medications for intrathecal administration include analgesics such as morphine and baclofen for pain and spasticity management, as well as chemotherapeutic agents like methotrexate for central nervous system malignancies. Subdural administration is less common but may involve corticosteroids or anesthetics used during neurosurgical procedures to reduce inflammation and provide localized pain control. Both routes require precise dosing and monitoring to avoid neurotoxic effects and ensure therapeutic efficacy.
Clinical Applications and Therapeutic Uses
Intrathecal administration involves injecting medication directly into the cerebrospinal fluid within the subarachnoid space, commonly used for spinal anesthesia, chemotherapy, and pain management in chronic conditions. Subdural injections deliver drugs into the potential space between the dura mater and arachnoid mater, primarily utilized for diagnostic imaging and targeted treatment of subdural hematomas or infections. Intrathecal therapy offers rapid central nervous system drug delivery with high bioavailability, while subdural approaches provide localized treatment with reduced systemic exposure.
Risks and Complications: Intrathecal vs Subdural
Intrathecal administration carries risks such as infection, bleeding, nerve damage, and potential for severe headaches due to cerebrospinal fluid leakage. Subdural injections pose complications including hematoma formation, neurological deficits, and challenges in accurate catheter placement leading to ineffective drug delivery. Both methods require careful monitoring to mitigate risks of paralysis, seizures, and other serious adverse effects linked to their proximity to the spinal cord and meninges.
Diagnostic Uses in Neurology and Anesthesia
Intrathecal injections deliver medication directly into the cerebrospinal fluid (CSF), enabling precise diagnostic evaluation of central nervous system conditions such as meningitis or multiple sclerosis via cerebrospinal fluid analysis. Subdural injections, placed between the dura mater and arachnoid membrane, are less commonly used diagnostically but may assist in identifying epidural space abnormalities or localized spinal pathologies through contrast-enhanced imaging techniques. In anesthesia, intrathecal administration offers rapid onset and profound sensory blockade crucial for spinal anesthesia, whereas subdural injections provide intermediate diffusion profiles useful in selective nerve root testing and pain diagnosis.
Patient Outcomes and Efficacy Comparison
Intrathecal drug delivery targets the cerebrospinal fluid in the subarachnoid space, providing rapid onset and effective pain relief, especially in chronic pain and spasticity management, with lower systemic side effects. Subdural administration, positioned between the dura mater and arachnoid, yields slower onset and less predictable drug dispersion, often resulting in variable efficacy and increased risk of neurological complications. Patient outcomes generally favor intrathecal approaches due to precise drug delivery and improved symptom control, supporting its preferred use in clinical pain management protocols.
Future Directions and Innovations
Intrathecal drug delivery systems are advancing with the integration of programmable pumps and sensor technologies enabling precise dosing and real-time monitoring. Research on subdural catheter placements explores minimally invasive techniques combined with biomaterials to reduce infection risk and improve long-term stability. Emerging innovations include biodegradable drug reservoirs and wireless control systems to enhance patient compliance and therapeutic outcomes.
Intrathecal Infographic
 libterm.com
libterm.com