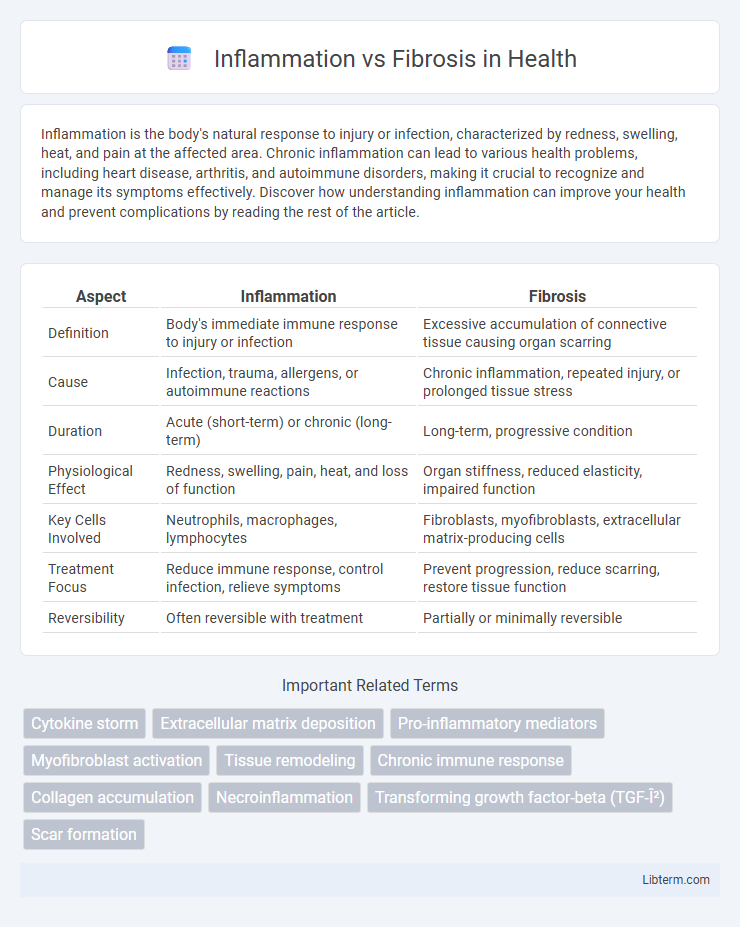
Inflammation is the body's natural response to injury or infection, characterized by redness, swelling, heat, and pain at the affected area. Chronic inflammation can lead to various health problems, including heart disease, arthritis, and autoimmune disorders, making it crucial to recognize and manage its symptoms effectively. Discover how understanding inflammation can improve your health and prevent complications by reading the rest of the article.
Table of Comparison
| Aspect | Inflammation | Fibrosis |
|---|---|---|
| Definition | Body's immediate immune response to injury or infection | Excessive accumulation of connective tissue causing organ scarring |
| Cause | Infection, trauma, allergens, or autoimmune reactions | Chronic inflammation, repeated injury, or prolonged tissue stress |
| Duration | Acute (short-term) or chronic (long-term) | Long-term, progressive condition |
| Physiological Effect | Redness, swelling, pain, heat, and loss of function | Organ stiffness, reduced elasticity, impaired function |
| Key Cells Involved | Neutrophils, macrophages, lymphocytes | Fibroblasts, myofibroblasts, extracellular matrix-producing cells |
| Treatment Focus | Reduce immune response, control infection, relieve symptoms | Prevent progression, reduce scarring, restore tissue function |
| Reversibility | Often reversible with treatment | Partially or minimally reversible |
Understanding Inflammation: Definition and Mechanisms
Inflammation is a complex biological response initiated by the immune system to harmful stimuli such as pathogens, damaged cells, or irritants, aiming to eliminate the initial cause of injury and initiate tissue repair. Key mechanisms involve the release of pro-inflammatory cytokines, activation of immune cells like macrophages and neutrophils, and increased vascular permeability allowing immune components to reach affected tissues. Understanding these processes is crucial for distinguishing between acute inflammation, which is protective, and chronic inflammation, which can lead to tissue damage and fibrosis.
What is Fibrosis? Causes and Progression
Fibrosis is the excessive accumulation of extracellular matrix proteins, including collagen, leading to tissue scarring and impaired organ function. It results from chronic inflammation caused by persistent injury, autoimmune diseases, infections, or environmental factors like toxins. Over time, fibrosis progresses through the activation of fibroblasts and myofibroblasts, which deposit collagen and disrupt normal tissue architecture, ultimately causing organ stiffness and failure.
Key Differences Between Inflammation and Fibrosis
Inflammation is an immediate immune response characterized by redness, swelling, and immune cell activation to eliminate pathogens or repair tissue damage, whereas fibrosis is a pathological process involving excessive accumulation of extracellular matrix proteins leading to scar tissue formation and organ dysfunction. Inflammation is typically reversible and resolves once the injury or infection is controlled, while fibrosis represents a chronic, irreversible remodeling phase often resulting in tissue stiffness. Key molecular mediators differ, with pro-inflammatory cytokines like TNF-a dominating inflammation and profibrotic factors such as TGF-b driving fibrosis progression.
The Role of Immune Cells in Inflammation and Fibrosis
Immune cells play a pivotal role in both inflammation and fibrosis by modulating tissue responses through cytokine secretion and cellular signaling pathways. During inflammation, macrophages and neutrophils infiltrate damaged tissue to clear pathogens and debris, while in fibrosis, activated macrophages and fibroblasts promote extracellular matrix deposition leading to scar tissue formation. The balance between pro-inflammatory immune signals and fibrotic responses determines the progression from acute injury to chronic tissue remodeling.
Acute vs Chronic Inflammation: Impact on Tissue Health
Acute inflammation triggers a rapid immune response that promotes tissue repair, while chronic inflammation leads to prolonged immune activation, resulting in fibrosis and compromised tissue function. Persistent inflammatory signals stimulate fibroblast proliferation and excessive extracellular matrix deposition, disrupting normal tissue architecture. Understanding the balance between acute and chronic inflammation is critical for preventing fibrotic diseases and preserving tissue health.
From Inflammation to Fibrosis: The Pathological Link
Chronic inflammation triggers a cascade of cellular events that activate fibroblasts, leading to excessive extracellular matrix deposition and tissue scarring known as fibrosis. Persistent inflammatory signals, particularly cytokines like TGF-b and IL-1b, drive fibroblast proliferation and myofibroblast differentiation, which are key mediators in fibrotic tissue remodeling. This pathological link between inflammation and fibrosis underlies many chronic diseases, including pulmonary fibrosis, liver cirrhosis, and systemic sclerosis, making the modulation of inflammatory pathways a critical target for therapeutic intervention.
Common Diseases Involving Both Inflammation and Fibrosis
Chronic diseases such as liver cirrhosis, idiopathic pulmonary fibrosis, and systemic sclerosis prominently feature both inflammation and fibrosis, where persistent inflammatory responses trigger excessive extracellular matrix deposition leading to tissue scarring. Inflammatory pathways involving cytokines like TGF-b and TNF-a play crucial roles in activating fibroblasts and promoting fibrotic remodeling. Effective treatment strategies target controlling inflammation to prevent progressive fibrosis and organ dysfunction in these conditions.
Diagnostic Markers for Inflammation and Fibrosis
Diagnostic markers for inflammation include elevated levels of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-a). In contrast, fibrosis is commonly identified through biomarkers like transforming growth factor-beta (TGF-b), collagen deposition markers including procollagen type III N-terminal peptide (PIIINP), and imaging techniques detecting tissue scarring. Differentiating inflammation from fibrosis relies on combining serological markers with histological analysis to assess active immune response versus extracellular matrix accumulation.
Treatment Strategies: Managing Inflammation and Preventing Fibrosis
Effective treatment strategies for managing inflammation and preventing fibrosis involve targeting key molecular pathways such as cytokines, TGF-b signaling, and oxidative stress. Anti-inflammatory agents like corticosteroids and NSAIDs reduce acute inflammation, while antifibrotic therapies including pirfenidone and nintedanib inhibit myofibroblast activation and extracellular matrix deposition. Early intervention with combination therapies that modulate immune responses and fibrotic processes shows promise in minimizing tissue damage and improving clinical outcomes.
Future Directions in Research on Inflammation and Fibrosis
Cutting-edge research is exploring molecular signaling pathways such as TGF-b and inflammasomes to develop targeted therapies for inflammation and fibrosis. Advances in single-cell RNA sequencing and spatial transcriptomics are unraveling cellular heterogeneity in fibrotic tissues, empowering precision medicine approaches. Emerging biomaterials and antifibrotic drugs are being tested in clinical trials to halt or reverse pathological tissue remodeling caused by chronic inflammation.
Inflammation Infographic
 libterm.com
libterm.com