A brain abscess is a serious medical condition characterized by a localized collection of pus within the brain tissue, usually caused by bacterial or fungal infections. Symptoms can include headache, fever, neurological deficits, and changes in mental status, requiring prompt diagnosis through imaging techniques like MRI or CT scans. Discover more about the causes, symptoms, treatment options, and prevention strategies to protect your brain health in the rest of this article.
Table of Comparison
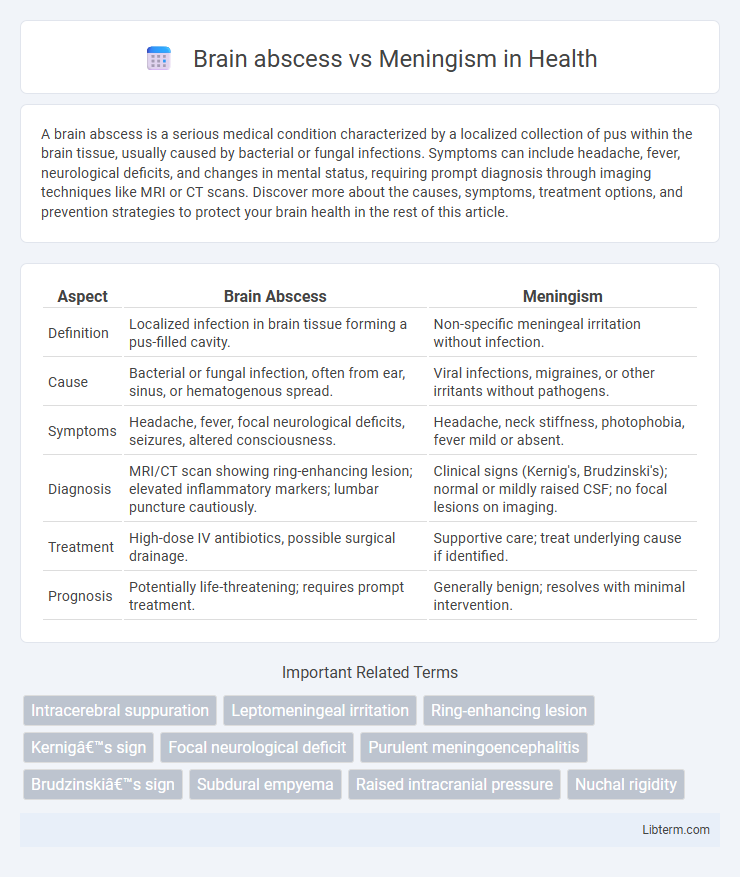
| Aspect | Brain Abscess | Meningism |
|---|---|---|
| Definition | Localized infection in brain tissue forming a pus-filled cavity. | Non-specific meningeal irritation without infection. |
| Cause | Bacterial or fungal infection, often from ear, sinus, or hematogenous spread. | Viral infections, migraines, or other irritants without pathogens. |
| Symptoms | Headache, fever, focal neurological deficits, seizures, altered consciousness. | Headache, neck stiffness, photophobia, fever mild or absent. |
| Diagnosis | MRI/CT scan showing ring-enhancing lesion; elevated inflammatory markers; lumbar puncture cautiously. | Clinical signs (Kernig's, Brudzinski's); normal or mildly raised CSF; no focal lesions on imaging. |
| Treatment | High-dose IV antibiotics, possible surgical drainage. | Supportive care; treat underlying cause if identified. |
| Prognosis | Potentially life-threatening; requires prompt treatment. | Generally benign; resolves with minimal intervention. |
Overview of Brain Abscess and Meningism
Brain abscess is a localized collection of pus within the brain parenchyma caused by bacterial or fungal infection, often resulting from contiguous spread, hematogenous dissemination, or direct inoculation. Meningism refers to a clinical syndrome characterized by signs of meningeal irritation, such as neck stiffness, photophobia, and headache, typically without actual inflammation of the meninges seen in meningitis. Differentiating brain abscess from meningism is critical, as brain abscess requires targeted antimicrobial therapy and may necessitate surgical intervention, whereas meningism often resolves once the underlying systemic cause is treated.
Etiology: Causes and Risk Factors
Brain abscess etiology primarily involves bacterial or fungal infections originating from contiguous spread, hematogenous dissemination, or direct inoculation, with common pathogens including Streptococcus, Staphylococcus aureus, and anaerobes; risk factors consist of immunosuppression, sinusitis, otitis media, and head trauma. Meningism arises from irritation of the meninges due to viral or bacterial infections, often seen in meningitis, with key pathogens being Neisseria meningitidis, Streptococcus pneumoniae, and enteroviruses; risk factors include close contact exposure, immunodeficiency, and recent upper respiratory infections. Differentiating these conditions requires understanding their distinct infectious sources and patient susceptibility profiles to guide targeted clinical management.
Pathophysiology Differences
Brain abscess results from a localized infection within the brain parenchyma leading to a pus-filled cavity due to bacterial or fungal invasion, often following contiguous spread or hematogenous dissemination. Meningism, characterized by irritation of the meninges without actual infection, involves inflammation secondary to conditions like viral illness or subarachnoid hemorrhage, causing meningeal irritation symptoms without purulent collection. The key pathophysiological difference lies in brain abscess causing focal intracerebral suppuration and mass effect, whereas meningism reflects meningeal inflammation without brain tissue involvement or abscess formation.
Clinical Presentation: Signs and Symptoms
Brain abscess typically presents with focal neurological deficits, severe headache, fever, and altered mental status, often accompanied by nausea, vomiting, and signs of increased intracranial pressure such as papilledema. Meningism commonly manifests with neck stiffness, photophobia, headache, and fever, without focal neurological signs, reflecting meningeal irritation rather than a localized brain lesion. Both conditions may share symptoms like headache and fever, but the presence of neurological deficits and signs of raised intracranial pressure favor a diagnosis of brain abscess.
Diagnostic Approaches and Key Findings
Brain abscess diagnosis relies on imaging techniques such as contrast-enhanced MRI and CT scans, revealing ring-enhancing lesions with central necrosis and surrounding edema. Cerebrospinal fluid (CSF) analysis in brain abscess may show elevated white blood cells and protein, but typically less pronounced than in meningism, where CSF demonstrates marked pleocytosis, increased protein, and decreased glucose levels indicative of meningeal inflammation. Clinical presentation differs, with brain abscess patients often exhibiting focal neurological deficits and raised intracranial pressure signs, while meningism is characterized by neck stiffness, photophobia, and headache, guiding differential diagnosis alongside laboratory and radiologic findings.
Neuroimaging: CT and MRI Features
Brain abscess on CT typically appears as a ring-enhancing lesion with central hypodensity, often accompanied by surrounding vasogenic edema and mass effect, while diffusion-weighted MRI shows restricted diffusion in the abscess core, which helps differentiate it from cystic tumors. In contrast, meningism, associated with meningeal irritation and inflammation, generally lacks focal intracranial lesions on CT or MRI, but may demonstrate meningeal enhancement, especially on contrast-enhanced MRI sequences. Neuroimaging thus plays a crucial role in distinguishing brain abscesses, which show characteristic localized abscess features, from meningism where imaging findings are either normal or reveal meningeal inflammation without abscess formation.
Laboratory Tests and CSF Analysis
Brain abscess typically presents with elevated white blood cell count, increased erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) in laboratory tests, while cerebrospinal fluid (CSF) analysis may reveal normal or mildly elevated protein and normal glucose levels without significant pleocytosis. Meningism, indicative of meningeal irritation without infection, usually shows normal laboratory inflammatory markers and CSF analysis, characterized by normal cell count, protein, and glucose levels. Differentiating these conditions relies on CSF findings combined with blood tests, where brain abscess manifests inflammatory responses absent in meningism.
Management and Treatment Strategies
Brain abscess treatment requires prompt antibiotic therapy tailored to the causative organisms, often combined with neurosurgical intervention such as aspiration or excision to reduce intracranial pressure and remove the infected material. Meningism management focuses on symptomatic relief, including analgesics and anti-inflammatory medications, while closely monitoring for potential progression to meningitis, which demands immediate antibiotic administration. Early differentiation between these conditions using imaging and clinical assessment guides appropriate treatment to prevent neurological complications.
Prognosis and Potential Complications
Brain abscess carries a higher risk of serious complications such as increased intracranial pressure, seizures, and neurological deficits, with prognosis heavily dependent on early diagnosis and effective antibiotic or surgical treatment. Meningism, characterized by symptoms similar to meningitis without actual infection or inflammation of the meninges, typically has a benign prognosis and rarely leads to long-term complications. Delayed recognition or misdiagnosis of brain abscess can result in life-threatening outcomes, while meningism usually resolves without sequelae.
Preventive Measures and Patient Education
Brain abscess prevention involves maintaining good hygiene, timely treatment of ear or sinus infections, and controlling immunosuppressive conditions to reduce infection risk. Educating patients on early symptoms such as headache, fever, and neurological deficits promotes prompt medical evaluation and antibiotic therapy. Meningism prevention emphasizes vaccination, avoiding close contact with infected individuals, and recognizing signs like neck stiffness and photophobia for early intervention.
Brain abscess Infographic
 libterm.com
libterm.com