Neutrophilia refers to an elevated number of neutrophils in the blood, often indicating infection, inflammation, or stress response. Common causes include bacterial infections, acute inflammation, and certain medications triggering bone marrow stimulation. Explore the rest of this article to understand how neutrophilia impacts your health and its diagnostic significance.
Table of Comparison
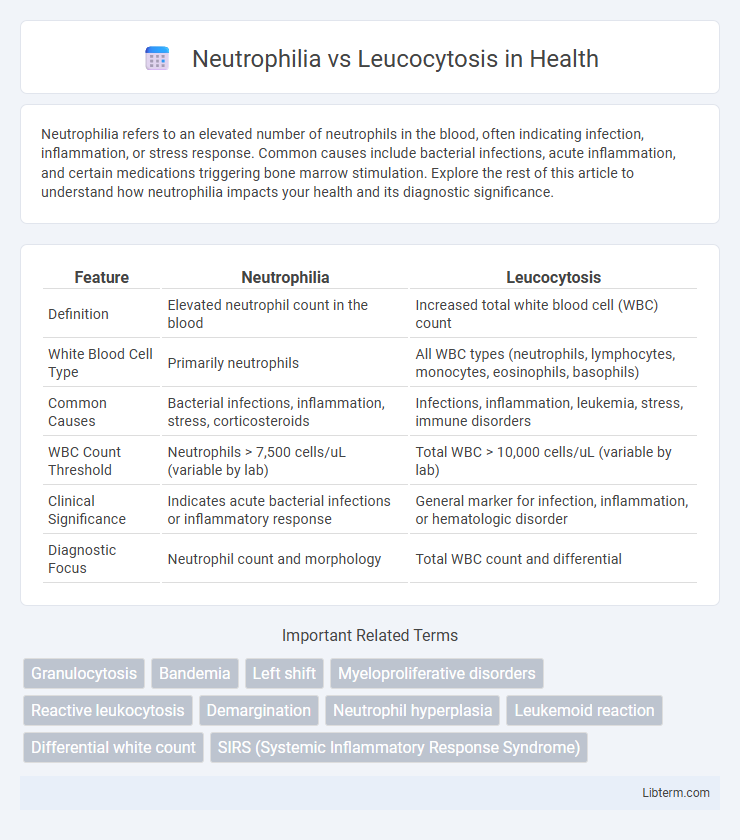
| Feature | Neutrophilia | Leucocytosis |
|---|---|---|
| Definition | Elevated neutrophil count in the blood | Increased total white blood cell (WBC) count |
| White Blood Cell Type | Primarily neutrophils | All WBC types (neutrophils, lymphocytes, monocytes, eosinophils, basophils) |
| Common Causes | Bacterial infections, inflammation, stress, corticosteroids | Infections, inflammation, leukemia, stress, immune disorders |
| WBC Count Threshold | Neutrophils > 7,500 cells/uL (variable by lab) | Total WBC > 10,000 cells/uL (variable by lab) |
| Clinical Significance | Indicates acute bacterial infections or inflammatory response | General marker for infection, inflammation, or hematologic disorder |
| Diagnostic Focus | Neutrophil count and morphology | Total WBC count and differential |
Introduction to Neutrophilia and Leucocytosis
Neutrophilia refers to an increased number of neutrophils, a type of white blood cell essential for fighting bacterial infections, typically indicating an acute inflammatory response. Leucocytosis is a broader term describing an elevated total white blood cell count, which may involve neutrophils, lymphocytes, eosinophils, or other subtypes, reflecting various conditions such as infections, inflammation, or hematologic disorders. Differentiating between neutrophilia and leptocytosis is crucial for diagnosis and treatment, as neutrophilia specifically highlights neutrophil elevation while leucocytosis encompasses all white blood cell increases.
Definitions: Neutrophilia vs Leucocytosis
Neutrophilia is defined as an increased number of neutrophils, a specific type of white blood cell crucial for fighting bacterial infections. Leucocytosis refers to a general increase in the total white blood cell count, encompassing neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Both conditions indicate immune system activation but differ based on the specific white blood cell populations elevated.
Types of White Blood Cells Involved
Neutrophilia specifically involves an increased number of neutrophils, the most abundant type of white blood cells responsible for combating bacterial infections and inflammation. Leucocytosis refers to an overall elevated white blood cell count, which can include neutrophils, lymphocytes, monocytes, eosinophils, or basophils depending on the underlying cause. Understanding the specific white blood cell type elevated aids in diagnosing conditions such as bacterial infections (neutrophilia) or viral infections and allergic reactions (other types of leucocytosis).
Causes of Neutrophilia
Neutrophilia is characterized by an elevated neutrophil count, commonly caused by bacterial infections, inflammation, stress, and certain medications such as corticosteroids. Unlike leucocytosis, which denotes an overall increase in white blood cells including lymphocytes, monocytes, eosinophils, and basophils, neutrophilia specifically involves the neutrophil subset. Conditions such as acute bacterial infections, trauma, acute inflammation, and myeloproliferative disorders are primary causes driving neutrophilia.
Causes of Leucocytosis
Leucocytosis refers to an elevated white blood cell (WBC) count, often caused by infections, inflammation, stress, trauma, or hematologic malignancies such as leukemia. Neutrophilia, a subtype of leucocytosis, specifically denotes an increased number of neutrophils, typically triggered by bacterial infections, acute inflammation, or corticosteroid use. Understanding the underlying cause of leucocytosis helps in differentiating between reactive processes and malignant conditions.
Clinical Significance of Neutrophilia
Neutrophilia, characterized by an increased neutrophil count above the normal range of 1.5-8.0 x 10^9/L, often indicates acute bacterial infections, inflammation, or stress responses, serving as a key diagnostic marker in clinical settings. Unlike general leucocytosis, which refers to an elevated total white blood cell count encompassing neutrophils, lymphocytes, monocytes, eosinophils, and basophils, neutrophilia specifically highlights neutrophil-driven immune activation and can point to conditions such as sepsis, trauma, or hematologic disorders like chronic myeloid leukemia. Early detection of neutrophilia through complete blood count (CBC) tests aids clinicians in diagnosing infections, guiding antibiotic therapy, and monitoring treatment efficacy.
Clinical Significance of Leucocytosis
Leucocytosis indicates an elevated white blood cell count, often signaling infections, inflammation, trauma, or hematologic malignancies, making it a critical marker in clinical diagnostics. Neutrophilia, a subtype of leucocytosis characterized by an increased number of neutrophils, typically points to bacterial infections, stress responses, or myeloproliferative disorders. Recognizing leucocytosis helps clinicians assess disease severity, monitor treatment efficacy, and guide further diagnostic testing in various medical conditions.
Diagnostic Criteria and Laboratory Findings
Neutrophilia is characterized by an elevated absolute neutrophil count, typically exceeding 7,500 cells/mL in adults, indicating a response to bacterial infections, inflammation, or stress. Leukocytosis refers to an increased total white blood cell count, often above 11,000 cells/mL, encompassing elevations in neutrophils, lymphocytes, monocytes, eosinophils, or basophils, which can suggest infections, hematologic malignancies, or physiological stress. Laboratory findings in neutrophilia demonstrate a predominance of mature and band neutrophils, while leukocytosis requires differential white blood cell counting to identify the specific leukocyte subtype responsible for the increase.
Management and Treatment Approaches
Management of neutrophilia primarily targets underlying causes such as infections, inflammation, or myeloproliferative disorders, often involving antibiotics, anti-inflammatory drugs, or cytoreductive therapy. Treatment of leucocytosis depends on etiology, ranging from addressing infections with antimicrobials to managing hematologic malignancies through chemotherapy or targeted therapies. Monitoring white blood cell counts and symptoms guides therapy adjustments to prevent complications like tissue damage or leukostasis.
Prognostic Implications and Outcomes
Neutrophilia, characterized by an elevated neutrophil count, often indicates acute bacterial infections or inflammatory responses and is associated with worse prognostic outcomes in conditions like sepsis and myocardial infarction. Leucocytosis, a broader increase in total white blood cells including neutrophils, lymphocytes, and monocytes, reflects systemic immune activation and may have variable prognostic implications depending on the underlying cause, such as infections, malignancies, or hematologic disorders. Prognostic outcomes in neutrophilia tend to be more closely tied to infection severity and tissue damage, whereas leucocytosis requires contextual clinical assessment to determine its impact on patient prognosis.
Neutrophilia Infographic
 libterm.com
libterm.com