A true aneurysm occurs when all three layers of the arterial wall (intima, media, and adventitia) bulge outward, creating a localized dilation of the vessel. This condition can lead to serious complications if left untreated, including rupture or thrombosis. Discover more about the causes, symptoms, and treatment options for true aneurysms by reading the rest of the article.
Table of Comparison
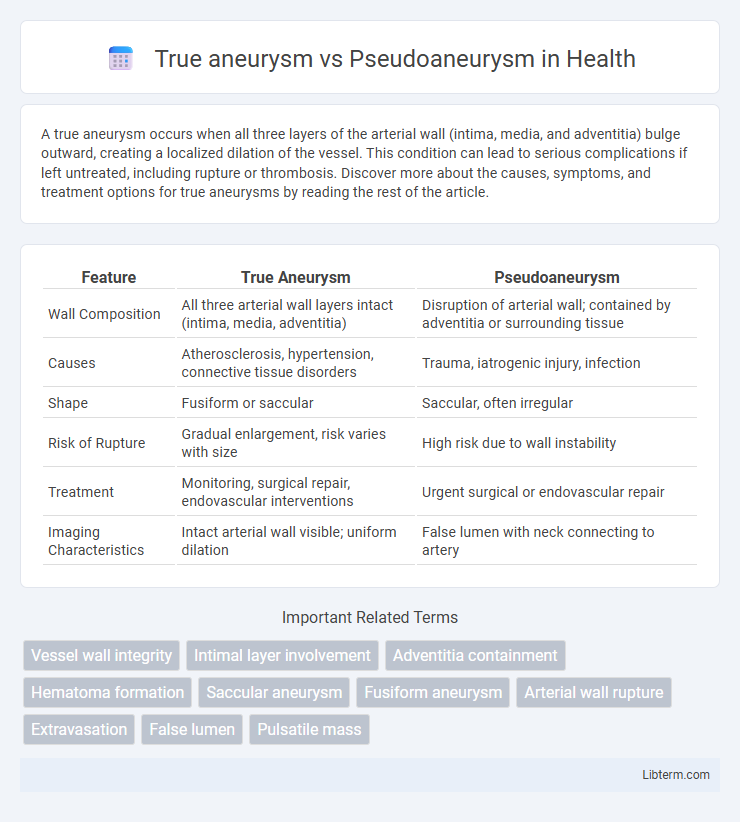
| Feature | True Aneurysm | Pseudoaneurysm |
|---|---|---|
| Wall Composition | All three arterial wall layers intact (intima, media, adventitia) | Disruption of arterial wall; contained by adventitia or surrounding tissue |
| Causes | Atherosclerosis, hypertension, connective tissue disorders | Trauma, iatrogenic injury, infection |
| Shape | Fusiform or saccular | Saccular, often irregular |
| Risk of Rupture | Gradual enlargement, risk varies with size | High risk due to wall instability |
| Treatment | Monitoring, surgical repair, endovascular interventions | Urgent surgical or endovascular repair |
| Imaging Characteristics | Intact arterial wall visible; uniform dilation | False lumen with neck connecting to artery |
Introduction to Aneurysms
True aneurysms involve the dilation of all three layers of the arterial wall, maintaining vessel wall integrity despite abnormal expansion. Pseudoaneurysms, or false aneurysms, occur when a vessel wall rupture leads to blood collection outside the arterial layers, contained by surrounding tissues. Differentiating between true and pseudoaneurysms is crucial for diagnosis and treatment planning due to their distinct pathophysiology and risk profiles.
Definition of True Aneurysm
A true aneurysm involves all three layers of the arterial wall--intima, media, and adventitia--resulting in a localized, permanent dilation of the blood vessel. This structural integrity distinguishes true aneurysms from pseudoaneurysms, which lack one or more arterial wall layers and are essentially contained ruptures. True aneurysms commonly occur in the aorta, cerebral arteries, and peripheral vessels, often linked to atherosclerosis or connective tissue disorders.
Definition of Pseudoaneurysm
A pseudoaneurysm, also known as a false aneurysm, occurs when there is a breach in the arterial wall causing blood to escape into the surrounding tissue, forming a contained hematoma that communicates with the arterial lumen. Unlike a true aneurysm, which involves all three layers of the arterial wall (intima, media, and adventitia), a pseudoaneurysm lacks an intact vessel wall and is instead enclosed by the surrounding connective tissue or perivascular structures. This structural difference is critical for diagnosis and treatment, as pseudoaneurysms often require intervention to prevent rupture and complications.
Key Differences: True vs Pseudoaneurysm
True aneurysms involve all three layers of the arterial wall--intima, media, and adventitia--resulting in a bulging vessel segment with an intact vessel wall structure. Pseudoaneurysms, or false aneurysms, occur when a blood vessel wall is injured and blood leaks into surrounding tissue, forming a pulsatile hematoma contained by the adventitia or perivascular tissue without involving all vessel wall layers. Key differences include the integrity of the vessel wall, with true aneurysms maintaining the wall structure while pseudoaneurysms lack a complete vessel wall, leading to higher rupture risk and different clinical management.
Etiology and Risk Factors
True aneurysms involve all three layers of the arterial wall and commonly result from atherosclerosis, hypertension, or genetic connective tissue disorders like Marfan syndrome. Pseudoaneurysms, or false aneurysms, occur due to a breach in the arterial wall causing blood to collect between the vessel layers, often resulting from trauma, iatrogenic injury, or infection. Risk factors for true aneurysms include chronic hypertension, smoking, and advanced age, while pseudoaneurysms frequently arise following vascular surgery, catheterization procedures, or penetrating injuries.
Pathophysiology and Structural Changes
True aneurysms involve all three layers of the arterial wall (intima, media, and adventitia) undergoing focal dilation due to weakening, often from atherosclerosis or genetic connective tissue disorders, resulting in a preserved but thinned vessel structure. Pseudoaneurysms, or false aneurysms, occur when a breach in the arterial wall leads to blood collecting outside the vessel layers, contained by the surrounding perivascular tissue rather than the vascular wall itself. This distinction in pathophysiology explains the difference in structural integrity, with true aneurysms retaining the vessel wall continuity and pseudoaneurysms lacking it, raising the risk of rupture.
Clinical Presentation and Symptoms
True aneurysms involve all three layers of the arterial wall and typically present with a pulsatile mass, localized pain, or are asymptomatic until rupture. Pseudoaneurysms, resulting from a breach in the arterial wall with blood contained by surrounding tissue, often present with rapid onset of swelling, tenderness, and possible bruit on auscultation. Both conditions may show signs of distal ischemia or neurological deficits depending on the aneurysm location.
Diagnostic Imaging Techniques
True aneurysms involve all three layers of the arterial wall and are typically identified using Doppler ultrasound and computed tomography angiography (CTA), which reveal a uniform dilation with an intact vessel wall. Pseudoaneurysms, or false aneurysms, result from a vessel wall rupture enclosed by surrounding tissues and are best visualized through color Doppler ultrasound showing a characteristic "yin-yang" flow pattern or contrast-enhanced CTA highlighting the extraluminal hematoma with a narrow neck. Magnetic resonance angiography (MRA) can further differentiate these lesions by providing detailed vessel wall imaging and flow dynamics essential for accurate diagnosis and treatment planning.
Treatment and Management Approaches
True aneurysms involve all three layers of the arterial wall and are often managed with surgical repair or endovascular stenting depending on size and risk of rupture, while pseudoaneurysms, characterized by a breach in arterial wall continuity and contained hematoma, typically require ultrasound-guided thrombin injection or surgical intervention if size or symptoms warrant. Endovascular approaches such as coil embolization or stent graft placement are increasingly preferred for pseudoaneurysms due to minimally invasive nature and reduced recovery time. Close imaging follow-up is essential for both conditions to monitor aneurysm stability and guide timely reintervention.
Prognosis and Complications
True aneurysms involve all three layers of the arterial wall, generally exhibiting a lower risk of rupture but a higher likelihood of progressive enlargement and thrombus formation, leading to potential embolic events. Pseudoaneurysms, characterized by a breach in the arterial wall with blood contained by surrounding tissues, possess a higher risk of rupture and rapid expansion, increasing the chances of hemorrhage and local tissue damage. Prognosis for true aneurysms is typically more favorable with timely surgical intervention, whereas pseudoaneurysms require urgent management to prevent life-threatening complications like rupture and compression of adjacent structures.
True aneurysm Infographic
 libterm.com
libterm.com