Hypercalcemia occurs when calcium levels in the blood exceed normal limits, potentially causing symptoms like fatigue, nausea, and confusion. Identifying the underlying causes, such as hyperparathyroidism or certain cancers, is crucial for effective treatment. Discover more about hypercalcemia's symptoms, causes, and management options in the full article.
Table of Comparison
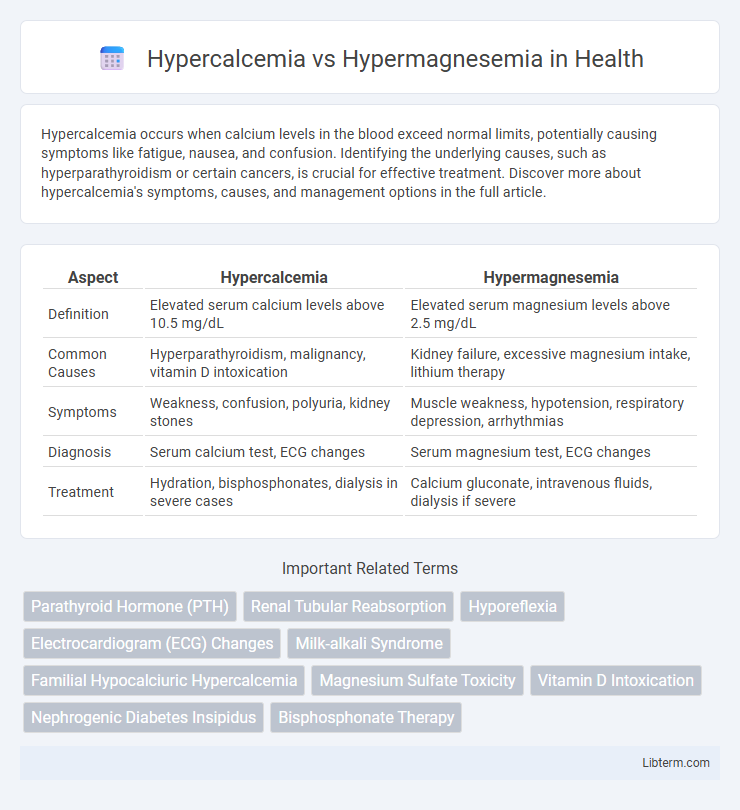
| Aspect | Hypercalcemia | Hypermagnesemia |
|---|---|---|
| Definition | Elevated serum calcium levels above 10.5 mg/dL | Elevated serum magnesium levels above 2.5 mg/dL |
| Common Causes | Hyperparathyroidism, malignancy, vitamin D intoxication | Kidney failure, excessive magnesium intake, lithium therapy |
| Symptoms | Weakness, confusion, polyuria, kidney stones | Muscle weakness, hypotension, respiratory depression, arrhythmias |
| Diagnosis | Serum calcium test, ECG changes | Serum magnesium test, ECG changes |
| Treatment | Hydration, bisphosphonates, dialysis in severe cases | Calcium gluconate, intravenous fluids, dialysis if severe |
Overview of Hypercalcemia and Hypermagnesemia
Hypercalcemia is characterized by elevated calcium levels above 10.5 mg/dL, often caused by hyperparathyroidism, malignancies, or excessive vitamin D intake, leading to symptoms like fatigue, kidney stones, and cardiac arrhythmias. Hypermagnesemia involves raised magnesium levels exceeding 2.5 mg/dL, frequently resulting from renal failure, magnesium-containing medications, or excessive supplementation, causing muscle weakness, hypotension, and respiratory depression. Both conditions disrupt electrolyte balance but differ in etiology, clinical manifestations, and treatment approaches.
Etiology and Causes of Hypercalcemia
Hypercalcemia primarily results from hyperparathyroidism, malignancies such as multiple myeloma or lung cancer, and excessive vitamin D intake, leading to increased calcium absorption and bone resorption. Other notable causes include granulomatous diseases like sarcoidosis, thiazide diuretics, and immobilization in patients with high bone turnover. In contrast, hypermagnesemia typically arises from renal failure, excessive magnesium administration, or antacid overuse, differentiating its etiology distinctly from the calcium imbalance seen in hypercalcemia.
Etiology and Causes of Hypermagnesemia
Hypermagnesemia primarily results from excessive magnesium intake, often due to renal failure, magnesium-containing medications, or laxatives, leading to impaired magnesium excretion. Etiologies include chronic kidney disease, adrenal insufficiency, and use of magnesium-based antacids or supplements. Unlike hypercalcemia, which is commonly caused by hyperparathyroidism or malignancy, hypermagnesemia is frequently linked to decreased renal clearance and iatrogenic magnesium overload.
Pathophysiological Differences
Hypercalcemia involves elevated serum calcium levels, typically resulting from increased bone resorption, excessive intestinal absorption, or decreased renal excretion, often linked to hyperparathyroidism or malignancies. Hypermagnesemia, characterized by elevated serum magnesium levels, frequently arises from impaired renal excretion or excessive magnesium intake, impacting neuromuscular and cardiovascular functions through calcium channel blockade. The distinct pathophysiological mechanisms highlight hypercalcemia's role in altering calcium-dependent signaling and bone metabolism, whereas hypermagnesemia primarily modulates cellular excitability and muscle contraction by affecting ion channel activity.
Clinical Manifestations: Signs and Symptoms
Hypercalcemia presents with symptoms such as fatigue, muscle weakness, polyuria, kidney stones, and neuropsychiatric disturbances including confusion and depression. Hypermagnesemia typically manifests as hypotension, bradycardia, muscle paralysis, diminished deep tendon reflexes, and respiratory depression. Both conditions require prompt recognition due to potential life-threatening cardiac arrhythmias and neuromuscular complications.
Diagnostic Strategies and Biomarkers
Hypercalcemia is diagnosed through serum calcium measurements, including corrected calcium and ionized calcium, alongside parathyroid hormone (PTH) levels to differentiate primary hyperparathyroidism from malignancy-related causes. Hypermagnesemia diagnosis involves serum magnesium concentration assessment, often paired with renal function tests and evaluation of electrolyte imbalances, particularly calcium and potassium levels. Biomarkers such as serum PTH help distinguish hypercalcemia etiologies, while elevated magnesium levels combined with electrolyte disturbances guide hypermagnesemia identification, emphasizing the importance of targeted biochemical panels in differential diagnosis.
Laboratory Findings: Key Distinctions
Hypercalcemia presents with elevated serum calcium levels typically above 10.5 mg/dL, often accompanied by decreased phosphate levels and increased parathyroid hormone or vitamin D metabolites depending on the etiology. In contrast, hypermagnesemia is characterized by serum magnesium concentrations exceeding 2.5 mg/dL, frequently linked with normal calcium and phosphate levels but may show decreased neuromuscular transmission on electrophysiological studies. Key distinctions in laboratory findings between the two include calcium and magnesium serum concentrations, parathyroid hormone activity, and phosphate levels, which guide accurate diagnosis and management.
Treatment Approaches for Hypercalcemia
Treatment approaches for hypercalcemia primarily involve hydration with intravenous saline to enhance renal calcium excretion, use of bisphosphonates to inhibit bone resorption, and calcitonin for rapid but short-term calcium reduction. In severe cases, corticosteroids may be employed to decrease calcium absorption, and dialysis is considered when renal failure complicates management. Management goals focus on addressing the underlying cause while carefully monitoring serum calcium levels and renal function.
Treatment Approaches for Hypermagnesemia
Hypermagnesemia treatment centers on discontinuing magnesium sources and administering intravenous calcium gluconate to counteract cardiac and neuromuscular effects. In severe cases, hemodialysis effectively removes excess magnesium from the bloodstream, especially when renal function is compromised. Supportive care includes fluid resuscitation and diuretics like furosemide to promote renal magnesium excretion.
Prognosis and Complications
Hypercalcemia often leads to complications such as nephrolithiasis, cardiac arrhythmias, and neurocognitive disturbances, with prognosis heavily dependent on underlying causes like malignancy or hyperparathyroidism. Hypermagnesemia usually results in neuromuscular depression, hypotension, and respiratory failure in severe cases, with prognosis improving upon prompt magnesium reduction and supportive care. Both conditions require careful monitoring of electrolyte levels to prevent life-threatening sequelae, though hypercalcemia tends to have a more variable and cause-specific prognosis.
Hypercalcemia Infographic
 libterm.com
libterm.com