Diarrhea is a common condition characterized by frequent, loose, or watery stools that can lead to dehydration and electrolyte imbalance if untreated. Understanding the causes, symptoms, and effective hydration techniques can help you manage and prevent complications. Explore the full article to learn practical tips for relief and when to seek medical attention.
Table of Comparison
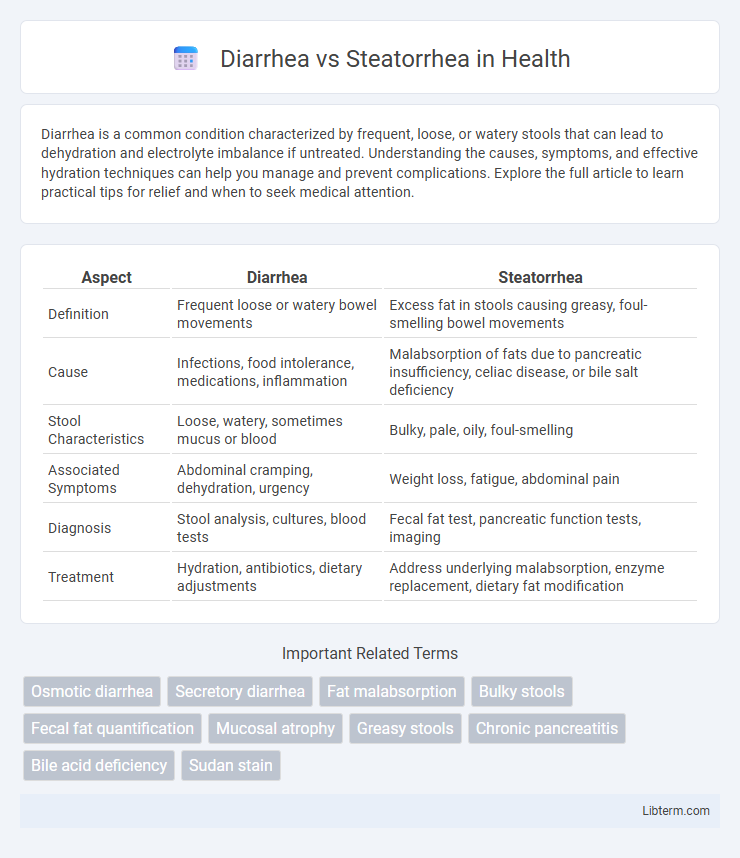
| Aspect | Diarrhea | Steatorrhea |
|---|---|---|
| Definition | Frequent loose or watery bowel movements | Excess fat in stools causing greasy, foul-smelling bowel movements |
| Cause | Infections, food intolerance, medications, inflammation | Malabsorption of fats due to pancreatic insufficiency, celiac disease, or bile salt deficiency |
| Stool Characteristics | Loose, watery, sometimes mucus or blood | Bulky, pale, oily, foul-smelling |
| Associated Symptoms | Abdominal cramping, dehydration, urgency | Weight loss, fatigue, abdominal pain |
| Diagnosis | Stool analysis, cultures, blood tests | Fecal fat test, pancreatic function tests, imaging |
| Treatment | Hydration, antibiotics, dietary adjustments | Address underlying malabsorption, enzyme replacement, dietary fat modification |
Understanding Diarrhea: Definition and Causes
Diarrhea is characterized by frequent, loose, or watery bowel movements resulting from increased intestinal motility or impaired absorption. Common causes include infections from viruses like rotavirus, bacterial pathogens such as Escherichia coli, or parasites; non-infectious causes involve food intolerances, inflammatory bowel disease, and certain medications. Understanding the underlying mechanisms of diarrhea helps differentiate it from steatorrhea, which involves fatty, malodorous stools due to malabsorption of fats rather than increased stool liquidity.
What is Steatorrhea? Key Features and Origins
Steatorrhea is characterized by the presence of excess fat in stools, leading to bulky, pale, and foul-smelling feces that often float due to high fat content. It primarily originates from malabsorption disorders such as pancreatic insufficiency, celiac disease, or bile salt deficiency, resulting in impaired fat digestion or absorption. Key features distinguishing steatorrhea from diarrhea include greasy stools and nutritional deficiencies linked to fat malabsorption rather than the watery consistency typical of diarrhea.
Core Differences: Diarrhea vs Steatorrhea
Diarrhea is characterized by frequent, loose, and watery bowel movements caused by infections, food intolerances, or malabsorption, leading to rapid transit of stool through the intestines. Steatorrhea involves bulky, pale, and foul-smelling stools that contain excess fat due to fat malabsorption from conditions such as pancreatic insufficiency, celiac disease, or bile acid deficiencies. The core difference lies in stool consistency and cause: diarrhea results from increased intestinal motility and fluid secretion, whereas steatorrhea reflects impaired fat digestion and absorption.
Common Symptoms: How They Present Clinically
Diarrhea typically presents with frequent, loose, and watery stools accompanied by abdominal cramps, urgency, and sometimes fever or dehydration. Steatorrhea manifests as bulky, pale, foul-smelling stools that float due to high fat content, often accompanied by weight loss, bloating, and malabsorption signs. Both conditions indicate underlying gastrointestinal disturbances but differ significantly in stool characteristics and associated systemic symptoms.
Underlying Medical Conditions Linked to Diarrhea
Persistent diarrhea is often linked to infections such as Giardia lamblia, Clostridium difficile, and viral gastroenteritis, as well as chronic conditions like inflammatory bowel disease (Crohn's disease and ulcerative colitis) and irritable bowel syndrome. Other underlying medical conditions include malabsorption syndromes like celiac disease and lactose intolerance, which disrupt nutrient absorption causing frequent loose stools. Identifying the cause typically requires stool analysis, blood tests, and sometimes endoscopic evaluation to distinguish diarrhea from steatorrhea, where fat malabsorption is a key feature.
Diseases and Disorders Associated with Steatorrhea
Steatorrhea is commonly associated with malabsorption disorders such as celiac disease, chronic pancreatitis, and cystic fibrosis, where fat digestion and absorption are impaired. Conditions like Crohn's disease and bile acid deficiency also lead to steatorrhea by disrupting normal lipid metabolism. Unlike typical diarrhea, steatorrhea is characterized by bulky, oily stools that indicate the presence of undigested fats.
Diagnostic Approaches: Identifying the Right Condition
Diagnostic approaches for diarrhea emphasize stool analysis, including frequency, consistency, and presence of infectious agents or blood, to differentiate infectious, inflammatory, or osmotic causes. Steatorrhea diagnosis relies on quantifying fat content in stool using fecal fat tests and Sudan staining, alongside pancreatic function tests and imaging to assess malabsorption syndromes. Advanced methods like breath tests for lactose intolerance or small intestinal bacterial overgrowth (SIBO) complement clinical evaluation to pinpoint the underlying disorder accurately.
Treatment Strategies: Diarrhea vs Steatorrhea
Treatment strategies for diarrhea primarily involve rehydration therapy using oral rehydration solutions, anti-motility agents like loperamide, and addressing underlying infections with antibiotics or antivirals. In contrast, steatorrhea treatment focuses on managing the underlying cause of malabsorption, such as pancreatic enzyme replacement therapy for pancreatic insufficiency or a gluten-free diet for celiac disease. Nutritional support with fat-soluble vitamin supplementation is crucial in steatorrhea to prevent deficiencies and promote intestinal healing.
Dietary Management Tips for Each Condition
Diarrhea management involves a diet rich in soluble fiber, such as oats and bananas, to help absorb excess water and reduce stool frequency, while avoiding greasy, spicy, and high-fat foods that can exacerbate symptoms. For steatorrhea, a low-fat diet combined with medium-chain triglycerides (MCTs) promotes fat absorption and minimizes fatty stools, and supplementation with fat-soluble vitamins (A, D, E, K) supports nutritional balance. Hydration is critical for both conditions to prevent dehydration, with attention to electrolyte replacement in diarrhea and enzyme supplementation in cases of pancreatic insufficiency related to steatorrhea.
When to Seek Medical Attention: Warning Signs
Seek medical attention for diarrhea if symptoms persist beyond 48 hours, are accompanied by high fever over 102degF (39degC), severe abdominal pain, or signs of dehydration such as dizziness and dark urine. For steatorrhea, medical evaluation is crucial when fatty, foul-smelling stools occur alongside unexplained weight loss, persistent abdominal discomfort, or signs of malnutrition like brittle hair or fatigue. Immediate care is necessary if there is blood in stools, persistent vomiting, or severe electrolyte imbalances, indicating potential underlying conditions.
Diarrhea Infographic
 libterm.com
libterm.com