Onychomycosis and lichen planus are distinct nail disorders that can cause discoloration, thickening, and damage to the nail plate, often leading to discomfort and cosmetic concerns. Onychomycosis is a fungal infection requiring antifungal treatments, while lichen planus is an inflammatory condition needing corticosteroids or immunosuppressants. Discover how to differentiate between these conditions and explore effective management strategies for maintaining your nail health in the rest of the article.
Table of Comparison
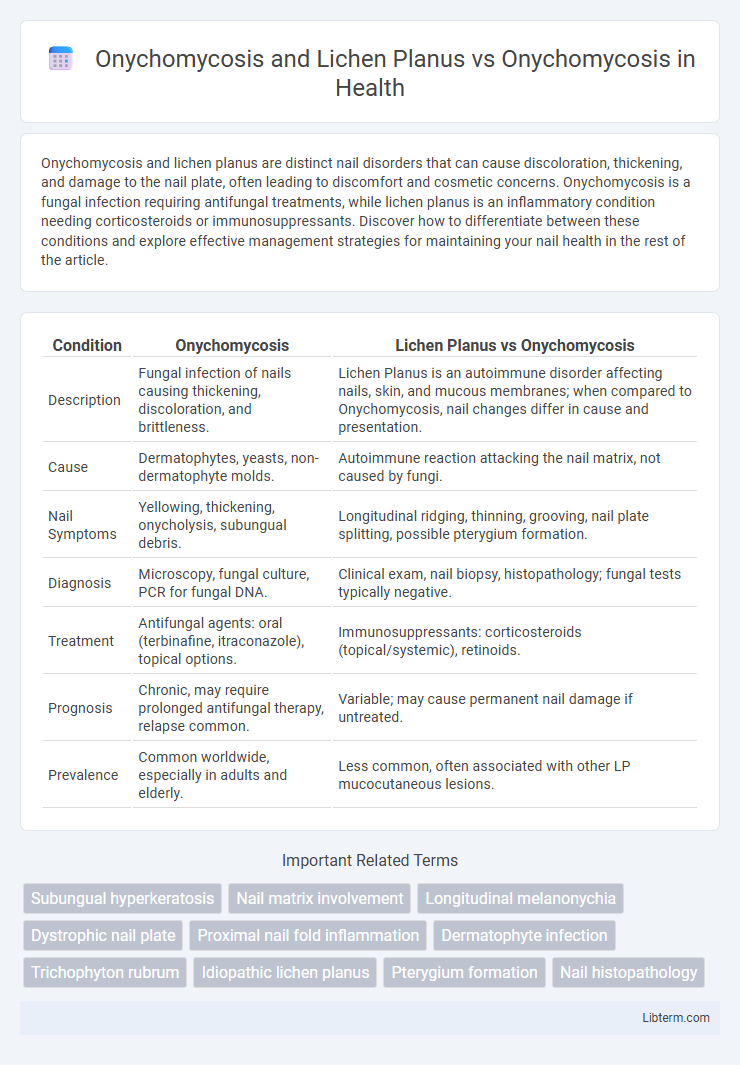
| Condition | Onychomycosis | Lichen Planus vs Onychomycosis |
|---|---|---|
| Description | Fungal infection of nails causing thickening, discoloration, and brittleness. | Lichen Planus is an autoimmune disorder affecting nails, skin, and mucous membranes; when compared to Onychomycosis, nail changes differ in cause and presentation. |
| Cause | Dermatophytes, yeasts, non-dermatophyte molds. | Autoimmune reaction attacking the nail matrix, not caused by fungi. |
| Nail Symptoms | Yellowing, thickening, onycholysis, subungual debris. | Longitudinal ridging, thinning, grooving, nail plate splitting, possible pterygium formation. |
| Diagnosis | Microscopy, fungal culture, PCR for fungal DNA. | Clinical exam, nail biopsy, histopathology; fungal tests typically negative. |
| Treatment | Antifungal agents: oral (terbinafine, itraconazole), topical options. | Immunosuppressants: corticosteroids (topical/systemic), retinoids. |
| Prognosis | Chronic, may require prolonged antifungal therapy, relapse common. | Variable; may cause permanent nail damage if untreated. |
| Prevalence | Common worldwide, especially in adults and elderly. | Less common, often associated with other LP mucocutaneous lesions. |
Overview of Onychomycosis
Onychomycosis is a common fungal infection affecting the nails, characterized by discoloration, thickening, and brittle or crumbly texture primarily caused by dermatophytes, yeasts, or non-dermatophyte molds. Unlike Lichen Planus, which is an inflammatory condition involving nail matrix damage and often causing longitudinal ridging or thinning, Onychomycosis results from fungal invasion disrupting the nail plate integrity. Accurate diagnosis through microscopy, culture, or molecular methods is essential for effective antifungal treatment and differentiation from similar nail disorders.
Understanding Lichen Planus in Nail Disorders
Lichen Planus in nail disorders presents with longitudinal ridging, thinning, and potential nail plate loss, which can be clinically confused with onychomycosis, a fungal infection characterized by nail discoloration, thickening, and subungual debris. Accurate differentiation is essential, as lichen planus is an inflammatory condition requiring immunomodulatory treatment, unlike onychomycosis, which necessitates antifungal therapy. Diagnostic tools such as nail biopsy and fungal culture or PCR aid in distinguishing lichen planus-induced nail changes from onychomycosis, ensuring targeted and effective management.
Key Differences: Onychomycosis vs Lichen Planus
Onychomycosis is a fungal infection primarily affecting the nail plate, characterized by discoloration, thickening, and brittleness, whereas Lichen Planus is an inflammatory autoimmune condition impacting the nail matrix, leading to longitudinal ridging, thinning, and nail loss. Diagnosis involves fungal culture or microscopy for Onychomycosis, while Lichen Planus requires clinical evaluation and biopsy to identify characteristic inflammatory infiltrates. Treatment differs significantly; Onychomycosis is managed with antifungal agents, whereas Lichen Planus often necessitates corticosteroids or immunosuppressive therapy.
Clinical Manifestations of Onychomycosis
Onychomycosis presents with thickened, brittle, and discolored nails, often showing subungual hyperkeratosis and onycholysis, predominantly affecting toenails. In contrast, Lichen Planus involves nail matrix inflammation leading to longitudinal ridging, thinning, and pterygium formation, distinct from fungal infection signs. Accurate diagnosis hinges on clinical examination complemented by mycological tests to differentiate onychomycosis from nail changes caused by Lichen Planus.
Nail Changes in Lichen Planus
Onychomycosis primarily causes nail thickening, discoloration, and subungual debris, whereas Lichen Planus induces distinctive nail changes such as longitudinal ridging, nail thinning, and pterygium formation. Nail matrix inflammation in Lichen Planus leads to scarring and permanent nail dystrophy, setting it apart from the fungal invasion in Onychomycosis. Recognizing Lichen Planus nail features is crucial for accurate diagnosis and differentiating from fungal nail infections, guiding appropriate treatment strategies.
Diagnostic Challenges: Onychomycosis and Lichen Planus
Onychomycosis and lichen planus both present with nail dystrophy, making differentiation challenging due to overlapping clinical features such as nail thickening, discoloration, and onycholysis. Accurate diagnosis requires a combination of direct microscopy, fungal cultures, and histopathological examination, as onychomycosis shows fungal invasion of the nail plate, whereas lichen planus reveals interface dermatitis with basal cell damage. Misdiagnosis can lead to inappropriate antifungal treatment, underscoring the importance of thorough diagnostic evaluation for effective management.
Laboratory Tests for Differentiation
Laboratory tests for differentiating Onychomycosis and Lichen Planus include direct microscopy with potassium hydroxide (KOH) preparation and fungal culture, which confirm Onychomycosis by detecting fungal elements. Nail biopsy with histopathological examination reveals lichenoid inflammation characteristic of Lichen Planus, helping exclude fungal infection. Polymerase chain reaction (PCR) assays provide sensitive fungal detection to differentiate Onychomycosis from nail changes caused by Lichen Planus.
Effective Management Strategies
Effective management of Onychomycosis involves antifungal agents such as terbinafine or itraconazole, with extended treatment durations to ensure eradication of the fungal infection. Lichen Planus affecting the nails requires corticosteroids, either topical or intralesional, to reduce inflammation and prevent permanent nail damage. Differentiating Onychomycosis from Lichen Planus is critical, as misdiagnosis can lead to inappropriate treatment and prolonged morbidity, highlighting the importance of precise diagnostic techniques like fungal cultures and biopsy.
Prognosis and Complications
Onychomycosis prognosis varies depending on the fungal species and treatment adherence, often requiring prolonged antifungal therapy for complete resolution, with complications including nail dystrophy and secondary bacterial infections. Lichen planus involving the nails presents a more challenging prognosis due to potential permanent nail loss, scarring, and irreversible nail matrix damage if untreated. Compared to onychomycosis, lichen planus complications tend to be more severe and may necessitate early intervention to prevent chronic nail deformities.
Prevention and Patient Education
Prevention of Onychomycosis involves maintaining proper nail hygiene, avoiding prolonged exposure to moisture, and using antifungal powders or sprays in high-risk environments. Patient education for Lichen Planus focuses on recognizing early symptoms such as nail ridging and discoloration to prevent secondary infections, while onychomycosis education emphasizes consistent treatment adherence to reduce fungal recurrence. Both conditions benefit from avoiding nail trauma and educating patients on the importance of regular dermatological evaluations for early detection and management.
Onychomycosis and Lichen Planus Infographic
 libterm.com
libterm.com