Hypercalcemia is a condition characterized by abnormally high levels of calcium in the blood, which can disrupt normal cellular function and lead to symptoms such as fatigue, nausea, and kidney stones. Causes often include overactive parathyroid glands, certain cancers, or excessive vitamin D intake, making timely diagnosis essential for effective management. Explore the detailed causes, symptoms, and treatment options to better understand how hypercalcemia might affect your health.
Table of Comparison
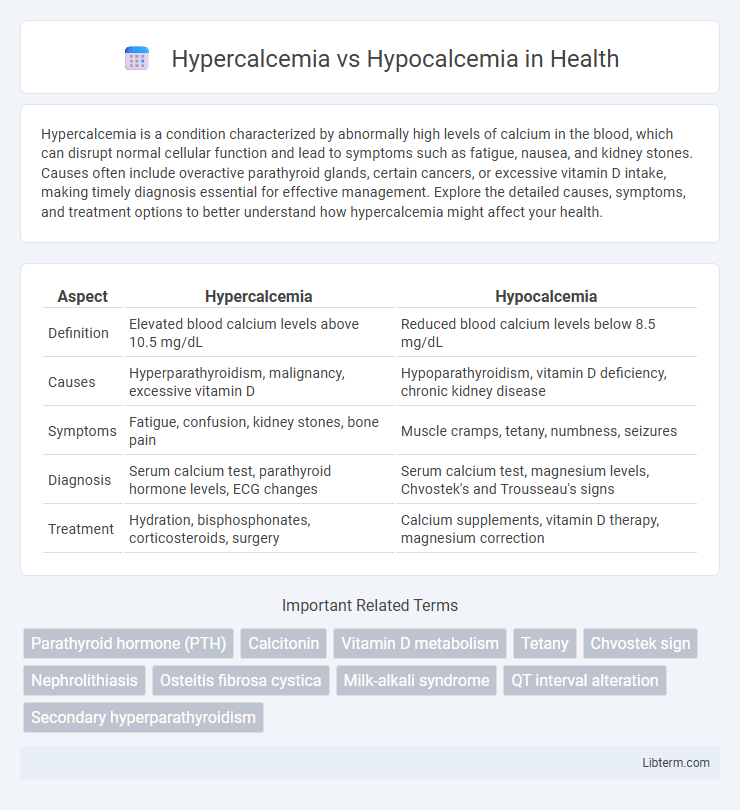
| Aspect | Hypercalcemia | Hypocalcemia |
|---|---|---|
| Definition | Elevated blood calcium levels above 10.5 mg/dL | Reduced blood calcium levels below 8.5 mg/dL |
| Causes | Hyperparathyroidism, malignancy, excessive vitamin D | Hypoparathyroidism, vitamin D deficiency, chronic kidney disease |
| Symptoms | Fatigue, confusion, kidney stones, bone pain | Muscle cramps, tetany, numbness, seizures |
| Diagnosis | Serum calcium test, parathyroid hormone levels, ECG changes | Serum calcium test, magnesium levels, Chvostek's and Trousseau's signs |
| Treatment | Hydration, bisphosphonates, corticosteroids, surgery | Calcium supplements, vitamin D therapy, magnesium correction |
Introduction to Calcium Homeostasis
Calcium homeostasis is tightly regulated by the parathyroid hormone (PTH), calcitonin, and vitamin D to maintain serum calcium levels between 8.5 and 10.5 mg/dL. Hypercalcemia occurs when serum calcium exceeds this range, often due to hyperparathyroidism or malignancy, whereas hypocalcemia results from insufficient calcium or vitamin D levels, hypoparathyroidism, or renal dysfunction. Proper calcium balance is crucial for neuromuscular function, bone health, and enzymatic activity.
What is Hypercalcemia?
Hypercalcemia is a condition characterized by abnormally high levels of calcium in the blood, typically above 10.5 mg/dL. It can result from hyperparathyroidism, malignancies, excessive vitamin D intake, or certain medications, leading to symptoms such as fatigue, kidney stones, and neurological disturbances. Accurate diagnosis involves serum calcium tests and identification of underlying causes to guide appropriate treatment and prevent complications.
What is Hypocalcemia?
Hypocalcemia is a medical condition characterized by abnormally low levels of calcium in the blood, often defined as serum calcium levels below 8.5 mg/dL. It commonly results from vitamin D deficiency, hypoparathyroidism, or chronic kidney disease, leading to symptoms like muscle cramps, tetany, and neurological disturbances. Understanding the causes and effects of hypocalcemia is crucial for effective diagnosis and treatment, distinguishing it from hypercalcemia, which involves elevated calcium levels.
Causes of Hypercalcemia
Hypercalcemia is primarily caused by hyperparathyroidism, malignancies such as multiple myeloma or lung cancer, and excessive vitamin D intake. Other causes include certain medications like thiazide diuretics and prolonged immobilization. In contrast, hypocalcemia generally results from hypoparathyroidism, vitamin D deficiency, or chronic kidney disease.
Causes of Hypocalcemia
Hypocalcemia is primarily caused by conditions that impair calcium absorption or metabolism, such as vitamin D deficiency, chronic kidney disease, and hypoparathyroidism. Other causes include magnesium deficiency, which affects parathyroid hormone secretion, and medications like bisphosphonates or anticonvulsants that alter calcium levels. Identifying underlying causes is critical for effective management and prevention of complications associated with low serum calcium.
Clinical Manifestations: Hypercalcemia vs Hypocalcemia
Hypercalcemia presents with clinical manifestations such as muscle weakness, polyuria, kidney stones, constipation, and cognitive disturbances including confusion or lethargy. Hypocalcemia typically manifests through neuromuscular irritability including tetany, muscle cramps, paresthesias, and in severe cases, seizures or cardiac arrhythmias due to prolonged QT interval. Identifying the distinct symptoms of hypercalcemia and hypocalcemia aids in prompt diagnosis and targeted management.
Diagnostic Approaches for Calcium Imbalances
Diagnosing calcium imbalances involves serum calcium measurement, considering both total and ionized calcium levels for accuracy in hypercalcemia and hypocalcemia assessment. Supplementary tests such as parathyroid hormone (PTH) assays, vitamin D levels, and renal function tests help determine the underlying cause. Imaging studies like neck ultrasound or bone scans may be employed to identify parathyroid adenomas or metastatic bone disease in complex cases.
Treatment Strategies: Hypercalcemia vs Hypocalcemia
Treatment strategies for hypercalcemia primarily involve hydration with intravenous saline to promote renal calcium excretion, bisphosphonates to inhibit bone resorption, and addressing underlying causes such as malignancy or hyperparathyroidism. Hypocalcemia management emphasizes rapid calcium supplementation, typically with intravenous calcium gluconate for acute symptoms, alongside oral calcium and vitamin D analogs to maintain long-term calcium homeostasis. Monitoring serum calcium levels and correcting electrolyte imbalances are critical components in both conditions to prevent complications like cardiac arrhythmias or neuromuscular irritability.
Potential Complications of Untreated Calcium Disorders
Untreated hypercalcemia can lead to severe complications such as kidney stones, arrhythmias, and osteoporosis due to excessive calcium disrupting cellular functions and bone metabolism. Hypocalcemia, if left unmanaged, increases the risk of neuromuscular irritability, tetany, seizures, and cardiac abnormalities like prolonged QT interval. Both conditions necessitate prompt diagnosis and treatment to prevent irreversible organ damage and life-threatening outcomes.
Prevention and Long-Term Management
Preventing hypercalcemia involves maintaining balanced dietary calcium intake, regular monitoring of serum calcium levels, and managing underlying conditions such as hyperparathyroidism or malignancies. Hypocalcemia prevention centers on ensuring adequate vitamin D and calcium supplementation, especially in at-risk populations like postmenopausal women or those with chronic kidney disease. Long-term management of both disorders requires close collaboration with healthcare providers to adjust treatment plans, monitor biochemical markers, and prevent complications such as bone demineralization or cardiac arrhythmias.
Hypercalcemia Infographic
 libterm.com
libterm.com