Regeneration is the process by which living organisms replace or restore lost or damaged tissues, ensuring survival and functionality. This natural ability varies widely among species, with some capable of regenerating entire limbs or organs, while others have more limited healing capacities. Explore the article to discover how regeneration works and what it means for your health and future medical advancements.
Table of Comparison
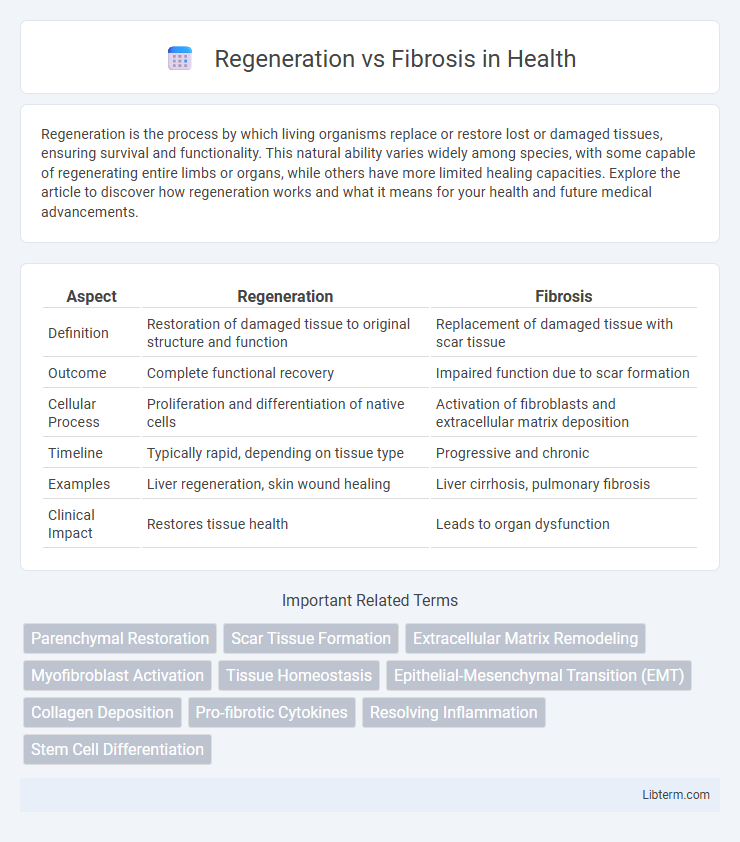
| Aspect | Regeneration | Fibrosis |
|---|---|---|
| Definition | Restoration of damaged tissue to original structure and function | Replacement of damaged tissue with scar tissue |
| Outcome | Complete functional recovery | Impaired function due to scar formation |
| Cellular Process | Proliferation and differentiation of native cells | Activation of fibroblasts and extracellular matrix deposition |
| Timeline | Typically rapid, depending on tissue type | Progressive and chronic |
| Examples | Liver regeneration, skin wound healing | Liver cirrhosis, pulmonary fibrosis |
| Clinical Impact | Restores tissue health | Leads to organ dysfunction |
Introduction to Tissue Healing: Regeneration vs Fibrosis
Tissue healing involves two primary processes: regeneration and fibrosis, which differ in outcomes and cellular mechanisms. Regeneration restores the original tissue architecture through proliferation of parenchymal cells, whereas fibrosis replaces damaged tissue with scar matrix due to excessive extracellular matrix deposition by activated fibroblasts. Understanding the balance between regeneration and fibrosis is crucial in developing therapeutic strategies for chronic wounds, organ injury, and fibrotic diseases.
Defining Regeneration: Restoring Normal Structure and Function
Regeneration involves the precise restoration of damaged tissues by replacing lost cells with identical ones, thereby reestablishing normal structure and function without scar formation. Unlike fibrosis, which leads to permanent scar tissue and impaired organ performance, regeneration maintains tissue integrity and physiological activity. Key molecular signals such as growth factors and extracellular matrix components orchestrate cellular proliferation and differentiation during the regenerative process.
Understanding Fibrosis: The Scarring Process
Fibrosis is the pathological accumulation of extracellular matrix components, primarily collagen, leading to tissue scarring and impaired organ function. It occurs when the normal wound healing process is disrupted, causing excessive fibroblast activation and myofibroblast differentiation. Persistent inflammation and signaling pathways such as TGF-b play key roles in driving fibrotic tissue remodeling and the loss of regenerative capacity.
Cellular and Molecular Mechanisms of Regeneration
Regeneration involves precise activation of signaling pathways such as Wnt, Notch, and Hedgehog to promote stem cell proliferation and differentiation, restoring tissue architecture and function. Cellular mechanisms include dedifferentiation of mature cells, activation of resident stem cells, and recruitment of progenitor cells that orchestrate repair through controlled extracellular matrix remodeling. Molecular factors like growth factors (FGF, TGF-b), cytokines, and matrix metalloproteinases regulate the balance between regeneration and fibrosis by modulating inflammation and tissue remodeling dynamics.
Key Pathways Involved in Fibrosis Development
Fibrosis development primarily involves the activation of the Transforming Growth Factor-beta (TGF-b) signaling pathway, which promotes fibroblast proliferation and extracellular matrix (ECM) deposition. The Wnt/b-catenin pathway also plays a critical role by regulating fibroblast differentiation and collagen synthesis. Additionally, the Platelet-Derived Growth Factor (PDGF) and Connective Tissue Growth Factor (CTGF) pathways contribute to the persistence of fibrotic tissue by sustaining myofibroblast activity and ECM accumulation.
Factors Influencing Regenerative Capacity
Regenerative capacity is influenced by factors such as the type of tissue, the presence of stem cells, and the local microenvironment, including extracellular matrix composition and signaling molecules like growth factors. Age and species differences also play crucial roles, with younger organisms and certain animals exhibiting higher regenerative potential due to more active cellular proliferation and differentiation pathways. Moreover, inflammation modulates the balance between regeneration and fibrosis, where controlled inflammation promotes tissue repair while chronic or excessive inflammation leads to fibroblast activation and scar formation.
Clinical Consequences of Fibrosis in Human Diseases
Fibrosis results in excessive accumulation of extracellular matrix components, leading to tissue scarring and impaired organ function in diseases such as liver cirrhosis, pulmonary fibrosis, and chronic kidney disease. The stiffening and loss of elasticity caused by fibrotic tissue contribute to organ failure, increased morbidity, and mortality in affected patients. Targeting fibrotic pathways remains a critical therapeutic strategy to prevent progression and improve clinical outcomes in fibrotic disorders.
Therapies Targeting Regeneration Over Fibrosis
Therapies targeting regeneration over fibrosis aim to promote tissue repair by activating stem cells and modulating extracellular matrix remodeling to restore normal tissue architecture. Recent advances include the use of growth factors, such as fibroblast growth factor (FGF) and transforming growth factor-beta (TGF-b) inhibitors, which suppress fibrotic pathways while enhancing regenerative signaling. Emerging cell-based therapies, including mesenchymal stem cell (MSC) applications, demonstrate reduced scar formation and improved functional recovery by shifting the balance towards regeneration rather than fibrosis.
Current Research Trends in Tissue Healing
Current research trends in tissue healing emphasize the molecular pathways differentiating regeneration and fibrosis, with a focus on manipulating signaling molecules like TGF-b and Wnt/b-catenin to promote regenerative outcomes. Advanced biomaterials and stem cell therapies are being developed to create microenvironments that favor tissue regeneration over fibrotic scarring. Cutting-edge genomic and proteomic analyses are identifying key regulators that can be targeted to enhance healing quality and reduce pathological fibrosis in organs such as the liver, heart, and skin.
Future Directions: Enhancing Regeneration, Preventing Fibrosis
Future directions in regenerative medicine emphasize molecular targeting to enhance tissue regeneration by modulating stem cell niches and extracellular matrix remodeling. Advances in biomaterials and gene editing technologies aim to promote functional tissue restoration while preventing fibrosis through precise control of inflammatory pathways and fibroblast activity. Integration of personalized medicine approaches holds promise for tailored therapies that shift the balance from fibrosis toward regeneration in chronic injury contexts.
Regeneration Infographic
 libterm.com
libterm.com