Urolithiasis significantly increases the risk of urinary tract infections (UTIs) due to obstruction and urinary stasis caused by kidney stones. These infections can escalate into severe complications if not promptly diagnosed and treated. Discover how understanding the link between urolithiasis and UTI can help protect your urinary health by reading the full article.
Table of Comparison
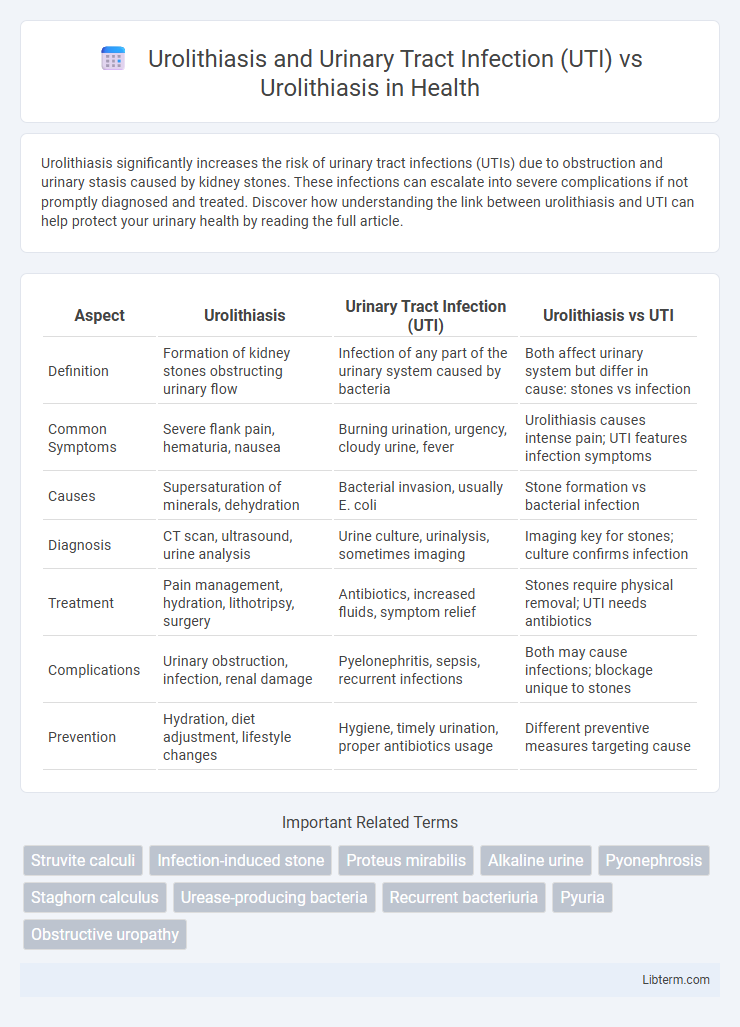
| Aspect | Urolithiasis | Urinary Tract Infection (UTI) | Urolithiasis vs UTI |
|---|---|---|---|
| Definition | Formation of kidney stones obstructing urinary flow | Infection of any part of the urinary system caused by bacteria | Both affect urinary system but differ in cause: stones vs infection |
| Common Symptoms | Severe flank pain, hematuria, nausea | Burning urination, urgency, cloudy urine, fever | Urolithiasis causes intense pain; UTI features infection symptoms |
| Causes | Supersaturation of minerals, dehydration | Bacterial invasion, usually E. coli | Stone formation vs bacterial infection |
| Diagnosis | CT scan, ultrasound, urine analysis | Urine culture, urinalysis, sometimes imaging | Imaging key for stones; culture confirms infection |
| Treatment | Pain management, hydration, lithotripsy, surgery | Antibiotics, increased fluids, symptom relief | Stones require physical removal; UTI needs antibiotics |
| Complications | Urinary obstruction, infection, renal damage | Pyelonephritis, sepsis, recurrent infections | Both may cause infections; blockage unique to stones |
| Prevention | Hydration, diet adjustment, lifestyle changes | Hygiene, timely urination, proper antibiotics usage | Different preventive measures targeting cause |
Introduction to Urolithiasis
Urolithiasis involves the formation of calculi or stones within the urinary tract, primarily affecting the kidneys, ureters, or bladder, and is characterized by pain, hematuria, and potential obstruction. Urinary Tract Infection (UTI) frequently coexists with urolithiasis due to urinary stasis and mucosal irritation caused by stones, complicating diagnosis and treatment. Understanding the pathophysiology of urolithiasis, including stone composition and risk factors like dehydration and metabolic disorders, is essential for effective clinical management and prevention of recurrent episodes.
Overview of Urinary Tract Infections (UTIs)
Urinary Tract Infections (UTIs) are bacterial infections affecting any part of the urinary system, most commonly the bladder and urethra, and frequently complicate cases of urolithiasis. Urolithiasis, characterized by the formation of kidney stones, increases the risk of UTIs by causing urinary obstruction and stasis, which promote bacterial growth and infection. Effective management of UTIs in patients with urolithiasis requires prompt diagnosis and targeted antibiotic therapy to prevent recurrent infections and renal damage.
Pathophysiological Differences: Urolithiasis vs UTI
Urolithiasis involves the formation of crystalline concretions within the urinary tract due to supersaturation of stone-forming ions like calcium, oxalate, and uric acid, often leading to obstruction and localized tissue injury. In contrast, urinary tract infection (UTI) is caused by bacterial colonization, predominantly Escherichia coli, resulting in an inflammatory response characterized by mucosal edema, leukocyte infiltration, and cytokine release. The key pathophysiological difference lies in urolithiasis being a metabolic and mechanical disorder driven by mineral precipitation, whereas UTI is an infectious-inflammatory condition triggered by microbial invasion.
Causes and Risk Factors: Stones with and without Infection
Urolithiasis involves the formation of kidney stones primarily due to factors such as dehydration, high urinary calcium, and dietary influences, whereas urinary tract infections (UTIs) contribute to stone formation mainly through urea-splitting bacteria like Proteus mirabilis, which increase urine pH and promote struvite stone development. Stones formed in the presence of infection often contain magnesium ammonium phosphate, showing distinct biochemical characteristics compared to calcium oxalate or uric acid stones seen in sterile conditions. Risk factors for UTI-associated stones include recurrent infections, urinary stasis, and anatomical abnormalities, while metabolic imbalances and genetic predisposition predominantly influence stone formation without infection.
Clinical Presentation: Urolithiasis Alone vs Urolithiasis with UTI
Urolithiasis alone typically presents with severe flank pain, hematuria, and urinary urgency, caused by obstruction and irritation from stones. When combined with a urinary tract infection (UTI), clinical presentation often includes fever, chills, dysuria, and cloudy or foul-smelling urine, indicating systemic infection alongside obstruction. The coexistence of UTI with urolithiasis increases the risk of complications such as pyelonephritis and sepsis, necessitating prompt diagnosis and treatment.
Diagnostic Approaches: Distinguishing Urolithiasis and UTI
Diagnostic approaches for distinguishing urolithiasis from urinary tract infection (UTI) emphasize imaging techniques such as non-contrast helical CT scans, which provide high sensitivity and specificity for detecting urinary stones, unlike UTIs that primarily require urine culture and sensitivity testing for identification. Urinalysis aids in differentiation by revealing hematuria common in urolithiasis, whereas pyuria and bacteriuria are indicative of UTIs. Combining clinical presentation with serum markers, imaging, and microbiological analysis enhances accuracy in diagnosing and differentiating these conditions.
Treatment Strategies: Stone Management vs Infected Stones
Urolithiasis treatment strategies prioritize stone management through hydration, analgesics, and surgical interventions such as extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy for stone removal. When urolithiasis is complicated by urinary tract infection (UTI), management emphasizes prompt antibiotic therapy combined with urgent drainage of infected obstructed urinary systems to prevent sepsis. Infected stones require careful coordination between infection control and stone clearance to reduce morbidity and recurrence risks effectively.
Complications: Risks of Urolithiasis with Concurrent UTI
Urolithiasis complicated by concurrent urinary tract infection (UTI) significantly increases the risk of severe complications such as urosepsis, renal abscess formation, and obstructive pyelonephritis, leading to impaired renal function. Bacterial colonization on urinary calculi promotes persistent infection and inflammation, exacerbating tissue damage and hindering stone clearance. These intertwined pathologies demand prompt diagnosis and targeted antibiotic therapy combined with stone removal to prevent long-term morbidity and renal failure.
Prevention and Recurrence: Targeted Interventions
Targeted interventions for preventing urolithiasis recurrence include increased hydration, dietary modifications to reduce oxalate and sodium intake, and use of thiazide diuretics or citrate supplements based on stone composition. In contrast, prevention strategies for urinary tract infections (UTI) associated with urolithiasis emphasize prompt stone removal, urinary acidification, and prophylactic antibiotics in recurrent cases. Integrating personalized medical management and lifestyle changes significantly lowers recurrence rates of both urolithiasis and UTI in affected patients.
Prognosis and Follow-up: Outcomes in Isolated vs Complicated Urolithiasis
Prognosis in isolated urolithiasis generally involves a lower risk of complications, with timely stone removal leading to favorable outcomes and minimal recurrence when follow-up includes regular imaging and metabolic evaluation. In cases complicated by Urinary Tract Infection (UTI), the prognosis worsens due to increased risks of sepsis, renal impairment, and recurrent stone formation, necessitating more aggressive antibiotic therapy and closer monitoring through urine cultures and renal function tests. Long-term follow-up in complicated urolithiasis requires a multidisciplinary approach to prevent chronic kidney disease and ensure early detection of infection-related complications.
Urolithiasis and Urinary Tract Infection (UTI) Infographic
 libterm.com
libterm.com