Dry eye syndrome occurs when your eyes do not produce enough tears or the tears evaporate too quickly, leading to discomfort and vision problems. Factors such as aging, environmental conditions, and prolonged screen time can exacerbate symptoms like redness, irritation, and a gritty sensation. Discover effective treatments and preventive strategies by reading the rest of this article.
Table of Comparison
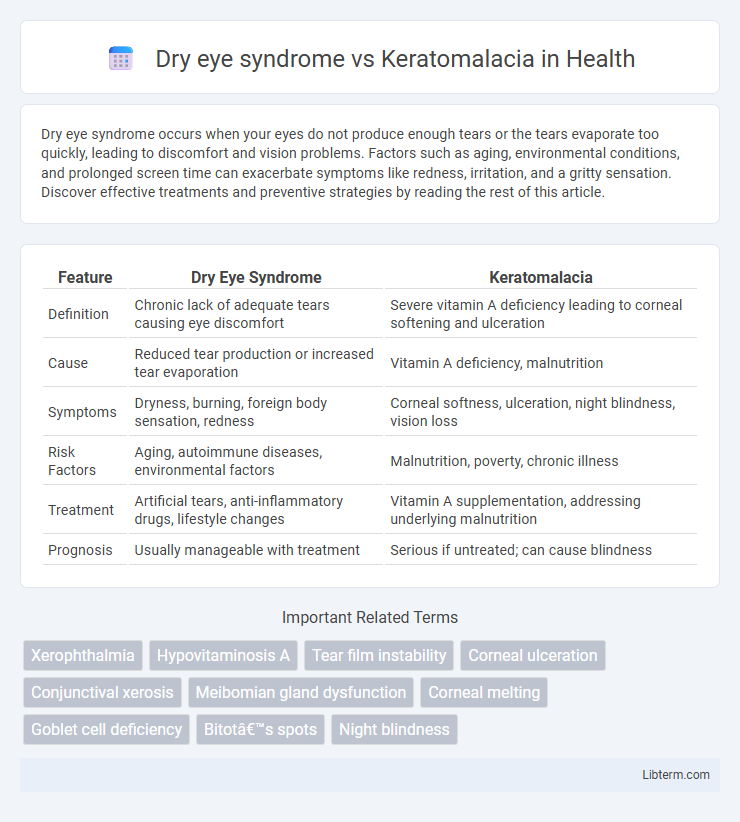
| Feature | Dry Eye Syndrome | Keratomalacia |
|---|---|---|
| Definition | Chronic lack of adequate tears causing eye discomfort | Severe vitamin A deficiency leading to corneal softening and ulceration |
| Cause | Reduced tear production or increased tear evaporation | Vitamin A deficiency, malnutrition |
| Symptoms | Dryness, burning, foreign body sensation, redness | Corneal softness, ulceration, night blindness, vision loss |
| Risk Factors | Aging, autoimmune diseases, environmental factors | Malnutrition, poverty, chronic illness |
| Treatment | Artificial tears, anti-inflammatory drugs, lifestyle changes | Vitamin A supplementation, addressing underlying malnutrition |
| Prognosis | Usually manageable with treatment | Serious if untreated; can cause blindness |
Understanding Dry Eye Syndrome
Dry eye syndrome is a common condition characterized by insufficient tear production or poor tear quality, leading to ocular surface dryness, irritation, and inflammation. Unlike keratomalacia, which results from severe vitamin A deficiency causing corneal softening and ulceration, dry eye syndrome primarily involves chronic tear film instability and hyperosmolarity. Effective management targets tear supplementation, anti-inflammatory therapies, and lifestyle modifications to restore ocular surface health and prevent complications.
What Is Keratomalacia?
Keratomalacia is a severe eye disorder characterized by the softening and ulceration of the cornea, primarily caused by vitamin A deficiency, leading to vision impairment and potentially blindness. Unlike dry eye syndrome, which involves inadequate tear production and ocular surface inflammation, keratomalacia results from a nutritional deficiency affecting corneal integrity. Early diagnosis and vitamin A supplementation are critical to prevent corneal damage and preserve visual function in keratomalacia patients.
Causes of Dry Eye Syndrome
Dry eye syndrome primarily arises from insufficient tear production or excessive tear evaporation caused by factors such as aging, hormonal changes, autoimmune diseases like Sjogren's syndrome, environmental conditions, and prolonged screen use. Meibomian gland dysfunction significantly contributes to evaporative dry eye by disrupting lipid layer stability, leading to tear film instability and ocular surface inflammation. Unlike keratomalacia, which results from severe vitamin A deficiency affecting corneal integrity, dry eye syndrome's underlying causes revolve around tear film instability and ocular surface abnormalities.
Causes of Keratomalacia
Keratomalacia primarily results from severe vitamin A deficiency, leading to corneal softening and ulceration, whereas dry eye syndrome stems from reduced tear production or increased tear evaporation. Vitamin A is essential for maintaining healthy corneal epithelium and mucous membranes, with deficiency often linked to malnutrition, malabsorption disorders, or chronic alcoholism. Early identification of keratomalacia's nutritional causes is critical to prevent irreversible vision loss.
Key Symptoms: Dry Eye vs Keratomalacia
Dry eye syndrome primarily presents with symptoms such as persistent eye dryness, irritation, a gritty or burning sensation, and occasional redness. Keratomalacia, associated with severe vitamin A deficiency, manifests through more severe symptoms including corneal softening, ulceration, and potential vision loss due to corneal melting or necrosis. While dry eye syndrome involves surface discomfort and tear film instability, keratomalacia leads to progressive corneal damage and poses a risk of blindness if untreated.
Risk Factors for Both Conditions
Dry eye syndrome primarily affects older adults and individuals with autoimmune diseases, prolonged screen exposure, or contact lens use, while Keratomalacia is strongly linked to severe vitamin A deficiency, often seen in malnourished children and populations with limited dietary access to vitamin A-rich foods. Environmental factors such as low humidity and pollution exacerbate dry eye risk, whereas Keratomalacia risk escalates in developing regions with high rates of malnutrition and infectious diseases like measles. Both conditions share immunocompromised states as a contributing factor but differ significantly in their underlying nutritional and environmental risk profiles.
Diagnostic Methods Compared
Dry eye syndrome diagnosis relies primarily on clinical tests such as the Schirmer test, tear breakup time (TBUT), and ocular surface staining with fluorescein or lissamine green to evaluate tear film quality and quantity. In contrast, keratomalacia diagnosis involves identifying vitamin A deficiency through serum retinol levels, alongside clinical examination revealing corneal softening, ulceration, and Bitot's spots. Imaging techniques like slit-lamp biomicroscopy are used in both but are crucial in keratomalacia to assess corneal integrity, while dry eye syndrome focuses more on tear film assessment.
Treatment Options: Dry Eye Syndrome
Dry eye syndrome treatment primarily involves artificial tears, lubricating eye drops, and lifestyle modifications to reduce eye strain and improve tear film stability. Prescription medications such as cyclosporine ophthalmic drops or lifitegrast eye drops target underlying inflammation to enhance tear production. In severe cases, punctal plugs or moisture chamber goggles may be utilized to conserve moisture and protect the ocular surface.
Treatment Options: Keratomalacia
Keratomalacia requires immediate vitamin A supplementation, often administered intramuscularly or orally, to halt corneal melting and restore ocular surface integrity. Intensive supportive care includes lubricating eye drops and antibiotics to prevent secondary infections, alongside managing underlying malnutrition to promote long-term recovery. In severe cases, surgical interventions like amniotic membrane transplantation or corneal grafting may be necessary to repair extensive corneal damage.
Preventive Measures and Prognosis
Dry eye syndrome prevention centers on maintaining ocular surface moisture through regular use of artificial tears, avoiding environmental triggers like wind and dry air, and addressing underlying conditions such as autoimmune diseases. Keratomalacia prevention requires adequate dietary intake of vitamin A, monitoring for malnutrition, and prompt treatment of vitamin A deficiency to avoid corneal softening and ulceration. Prognosis for dry eye syndrome is generally manageable with proper care, whereas keratomalacia can lead to permanent vision loss or blindness if untreated, highlighting the critical importance of early intervention.
Dry eye syndrome Infographic
 libterm.com
libterm.com