Cholecystitis is the inflammation of the gallbladder, often caused by gallstones blocking the cystic duct, leading to severe abdominal pain, fever, and digestive discomfort. Early diagnosis and treatment are crucial to prevent complications like gallbladder infection or rupture. Discover how you can recognize symptoms and explore effective treatment options in the rest of this article.
Table of Comparison
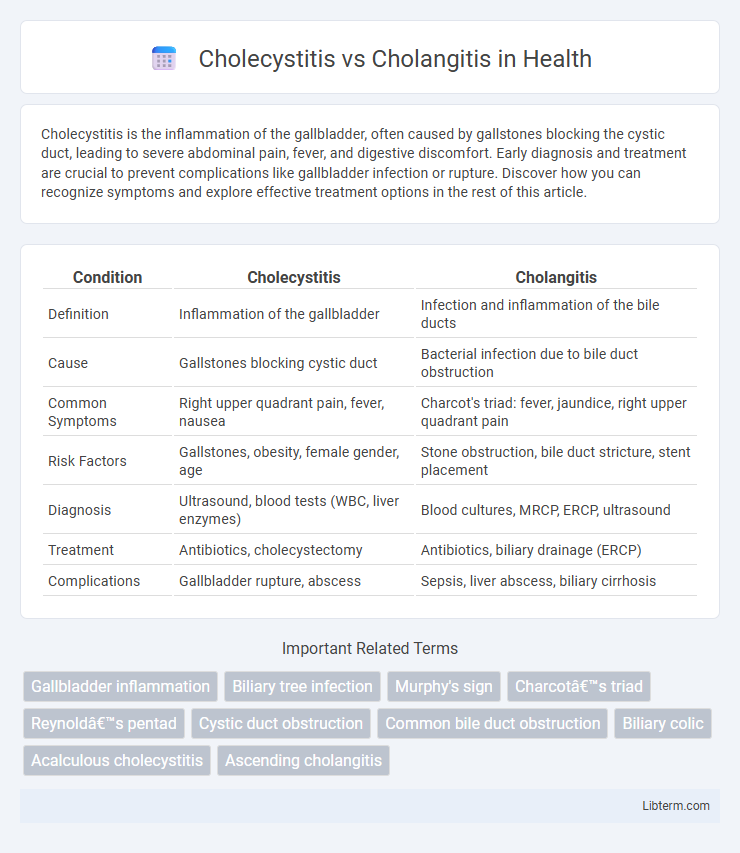
| Condition | Cholecystitis | Cholangitis |
|---|---|---|
| Definition | Inflammation of the gallbladder | Infection and inflammation of the bile ducts |
| Cause | Gallstones blocking cystic duct | Bacterial infection due to bile duct obstruction |
| Common Symptoms | Right upper quadrant pain, fever, nausea | Charcot's triad: fever, jaundice, right upper quadrant pain |
| Risk Factors | Gallstones, obesity, female gender, age | Stone obstruction, bile duct stricture, stent placement |
| Diagnosis | Ultrasound, blood tests (WBC, liver enzymes) | Blood cultures, MRCP, ERCP, ultrasound |
| Treatment | Antibiotics, cholecystectomy | Antibiotics, biliary drainage (ERCP) |
| Complications | Gallbladder rupture, abscess | Sepsis, liver abscess, biliary cirrhosis |
Introduction to Cholecystitis and Cholangitis
Cholecystitis is the inflammation of the gallbladder, often caused by gallstones obstructing the cystic duct, leading to pain and infection. Cholangitis is an infection of the bile ducts, usually resulting from bile duct obstruction due to stones, strictures, or tumors, causing fever, jaundice, and abdominal pain. Both conditions require prompt diagnosis and treatment to prevent severe complications such as sepsis or biliary cirrhosis.
Definition and Overview
Cholecystitis is the inflammation of the gallbladder, often caused by gallstones obstructing the cystic duct, leading to pain and infection. Cholangitis refers to infection and inflammation of the bile ducts, commonly resulting from bile duct obstruction, such as from gallstones, strictures, or tumors. Both conditions require prompt medical attention, but cholangitis typically presents with Charcot's triad: fever, jaundice, and right upper quadrant pain.
Etiology and Risk Factors
Cholecystitis primarily results from gallstone obstruction in the cystic duct, leading to inflammation of the gallbladder, with risk factors including obesity, female gender, age over 40, and rapid weight loss. Cholangitis is typically caused by bacterial infection due to bile duct obstruction from strictures, gallstones, or tumors, with risk factors such as bile duct injury, immunosuppression, and prior biliary surgery. Both conditions involve biliary stasis, but cholangitis presents a higher risk of systemic infection due to ascending bacterial invasion of the bile ducts.
Pathophysiology: Key Differences
Cholecystitis involves inflammation of the gallbladder, typically caused by gallstone obstruction of the cystic duct, leading to bile stasis, increased intraluminal pressure, and ischemia. Cholangitis results from bacterial infection and inflammation of the bile ducts, often due to bile duct obstruction from stones, strictures, or tumors, causing bile stasis and ascending infection. The key pathophysiological difference lies in cholecystitis affecting the gallbladder primarily, while cholangitis impacts the biliary tree's ductal system.
Clinical Presentation and Symptoms
Cholecystitis typically presents with right upper quadrant abdominal pain, fever, and tenderness, often accompanied by nausea and vomiting, reflecting inflammation of the gallbladder. Cholangitis manifests with Charcot's triad: fever, jaundice, and right upper quadrant pain, resulting from infection and obstruction of the bile ducts. Laboratory findings in cholangitis commonly show elevated bilirubin and liver enzymes, whereas cholecystitis primarily shows leukocytosis and localized inflammatory markers.
Diagnostic Approaches
Cholecystitis is typically diagnosed using abdominal ultrasound to detect gallbladder wall thickening, pericholecystic fluid, and gallstones, while laboratory tests often show elevated white blood cells and liver enzymes. Cholangitis diagnosis involves blood cultures and liver function tests indicating cholestasis, with imaging modalities like MRCP or ERCP identifying bile duct obstruction or strictures. Both conditions require targeted diagnostic approaches combining clinical presentation with specific imaging and lab results for accurate differentiation.
Radiological and Laboratory Findings
Cholecystitis typically presents with gallbladder wall thickening, pericholecystic fluid, and a sonographic Murphy sign on ultrasound, while laboratory findings often reveal elevated white blood cell count and mild elevations in liver enzymes such as alkaline phosphatase (ALP) and alanine aminotransferase (ALT). Cholangitis demonstrates bile duct dilation and sometimes biliary stones on imaging studies like ultrasound or MRCP (Magnetic Resonance Cholangiopancreatography), accompanied by significant elevations of cholestatic liver enzymes including ALP, gamma-glutamyl transferase (GGT), and bilirubin, alongside systemic signs of infection such as leukocytosis. Distinguishing features include elevated bilirubin and positive blood cultures frequently observed in cholangitis, whereas cholecystitis primarily shows localized inflammation without significant bilirubin elevation.
Treatment Strategies and Management
Cholecystitis treatment primarily involves antibiotics and cholecystectomy, focusing on inflammation of the gallbladder often caused by gallstones. Cholangitis management requires urgent biliary decompression through endoscopic retrograde cholangiopancreatography (ERCP) combined with broad-spectrum antibiotics targeting bile duct infection. Both conditions demand prompt intervention to prevent complications, but cholangitis necessitates more aggressive drainage procedures due to its life-threatening nature.
Complications and Prognosis
Cholecystitis can lead to severe complications such as gallbladder perforation, abscess formation, and sepsis if untreated, with a generally favorable prognosis following timely cholecystectomy. Cholangitis, often caused by bile duct obstruction, carries risks of biliary cirrhosis, sepsis, and multi-organ failure, demanding urgent antibiotic therapy and biliary decompression for improved outcomes. Mortality rates are higher in cholangitis due to its systemic involvement, whereas prompt surgical intervention in cholecystitis typically results in full recovery.
Prevention and Patient Education
Cholecystitis prevention emphasizes maintaining a low-fat diet and managing gallstones through regular medical check-ups to reduce inflammation of the gallbladder. Educating patients about recognizing early symptoms such as abdominal pain and fever helps ensure timely medical intervention. For cholangitis, prevention focuses on treating bile duct obstructions promptly and practicing good hygiene to avoid infections, while patient education highlights the importance of monitoring jaundice and seeking immediate care for fever and chills.
Cholecystitis Infographic
 libterm.com
libterm.com