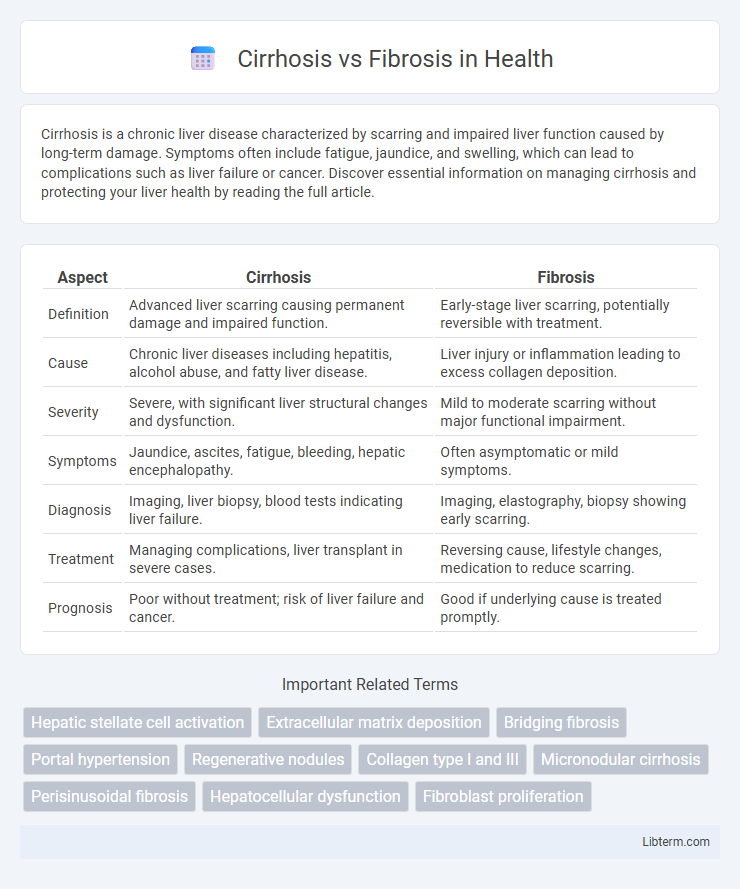
Cirrhosis is a chronic liver disease characterized by scarring and impaired liver function caused by long-term damage. Symptoms often include fatigue, jaundice, and swelling, which can lead to complications such as liver failure or cancer. Discover essential information on managing cirrhosis and protecting your liver health by reading the full article.
Table of Comparison
| Aspect | Cirrhosis | Fibrosis |
|---|---|---|
| Definition | Advanced liver scarring causing permanent damage and impaired function. | Early-stage liver scarring, potentially reversible with treatment. |
| Cause | Chronic liver diseases including hepatitis, alcohol abuse, and fatty liver disease. | Liver injury or inflammation leading to excess collagen deposition. |
| Severity | Severe, with significant liver structural changes and dysfunction. | Mild to moderate scarring without major functional impairment. |
| Symptoms | Jaundice, ascites, fatigue, bleeding, hepatic encephalopathy. | Often asymptomatic or mild symptoms. |
| Diagnosis | Imaging, liver biopsy, blood tests indicating liver failure. | Imaging, elastography, biopsy showing early scarring. |
| Treatment | Managing complications, liver transplant in severe cases. | Reversing cause, lifestyle changes, medication to reduce scarring. |
| Prognosis | Poor without treatment; risk of liver failure and cancer. | Good if underlying cause is treated promptly. |
Understanding Cirrhosis and Fibrosis
Cirrhosis and fibrosis are progressive liver conditions characterized by the accumulation of scar tissue due to chronic liver damage, but cirrhosis represents an advanced stage with extensive scarring disrupting liver architecture and function. Fibrosis is the initial response of the liver to injury, involving activation of hepatic stellate cells and deposition of extracellular matrix proteins, which can be reversible with early treatment. Understanding the molecular mechanisms and the extent of liver damage in fibrosis and cirrhosis is crucial for diagnosing severity and guiding therapeutic interventions to prevent liver failure and complications such as portal hypertension.
Key Differences Between Cirrhosis and Fibrosis
Cirrhosis is an advanced stage of liver fibrosis characterized by extensive scarring, nodular regeneration, and irreversible liver damage, whereas fibrosis refers to the initial accumulation of excess connective tissue due to chronic liver injury. Unlike fibrosis, cirrhosis significantly impairs liver function and often leads to complications such as portal hypertension and liver failure. Fibrosis can be reversible if the underlying cause is treated early, while cirrhosis is generally considered irreversible and requires more intensive management or liver transplantation.
Causes and Risk Factors
Cirrhosis and fibrosis both result from chronic liver damage, with fibrosis representing the initial scarring stage while cirrhosis is advanced liver scarring that impairs function. Key causes and risk factors include chronic hepatitis B or C infections, excessive alcohol consumption, non-alcoholic fatty liver disease (NAFLD), and autoimmune hepatitis. Genetic disorders like hemochromatosis and prolonged exposure to toxins or certain medications also contribute significantly to the progression from fibrosis to cirrhosis.
Stages of Liver Fibrosis
Liver fibrosis progresses through distinct stages labeled F0 to F4, with F0 indicating no fibrosis and F4 representing cirrhosis, the most advanced stage characterized by severe scarring and disrupted liver architecture. Early stages (F1-F2) show mild to moderate fibrotic tissue deposition without significant liver function impairment, while stage F3 denotes severe fibrosis with bridging scars. Accurate staging through liver biopsy or non-invasive elastography techniques is critical for prognosis and guiding treatment strategies in chronic liver diseases.
Progression From Fibrosis to Cirrhosis
Fibrosis represents the accumulation of scar tissue in the liver due to chronic injury, while cirrhosis is the advanced stage characterized by extensive fibrosis and nodular regeneration disrupting liver architecture. The progression from fibrosis to cirrhosis involves increased activation of hepatic stellate cells, persistent inflammation, and extracellular matrix deposition that impairs liver function. Early intervention targeting fibrosis can slow or prevent the development of cirrhosis, reducing the risk of complications like portal hypertension and liver failure.
Symptoms and Clinical Manifestations
Cirrhosis and fibrosis both involve liver scarring, but cirrhosis manifests with advanced symptoms such as jaundice, ascites, hepatic encephalopathy, and variceal bleeding, indicating significant liver dysfunction. Fibrosis, typically an earlier stage, presents with mild or no symptoms but may include fatigue and mild abdominal discomfort as liver tissue progressively scars. Clinical manifestations of cirrhosis include portal hypertension and coagulopathy, whereas fibrosis is often detected through imaging and biopsy before severe clinical signs develop.
Diagnosis: Tests and Imaging
Diagnosing cirrhosis versus fibrosis relies heavily on liver function tests, including serum aminotransferases (ALT, AST), bilirubin levels, and platelet counts, supplemented by imaging studies such as ultrasound elastography, CT scans, and MRI to assess liver texture and stiffness. Fibrosis staging often requires non-invasive elastography methods like transient elastography (FibroScan) or MR elastography to quantify scarring, while cirrhosis diagnosis is confirmed through characteristic nodular liver morphology and signs of portal hypertension observed in imaging. When non-invasive techniques are inconclusive, a liver biopsy remains the gold standard for differentiating between advanced fibrosis and established cirrhosis.
Treatment Options for Fibrosis and Cirrhosis
Treatment options for liver fibrosis primarily include antiviral medications, lifestyle changes such as alcohol cessation, and managing underlying conditions like hepatitis or fatty liver disease to prevent progression. Cirrhosis treatment focuses on addressing complications through diuretics for fluid retention, beta-blockers to reduce portal hypertension, and in advanced cases, liver transplantation as the definitive solution. Emerging therapies targeting fibrosis reversal are under clinical investigation but are not yet standard care for either condition.
Prevention and Lifestyle Modifications
Preventing cirrhosis and fibrosis primarily involves reducing risk factors such as chronic alcohol consumption, viral hepatitis infections, and obesity-related liver damage. Lifestyle modifications like maintaining a balanced diet rich in antioxidants, engaging in regular physical activity, and avoiding hepatotoxic substances significantly slow disease progression. Regular medical screenings and vaccinations for hepatitis B and C enhance early detection and prevention of liver scarring.
Prognosis and Long-Term Outcomes
Cirrhosis represents an advanced stage of liver fibrosis characterized by extensive scarring and impaired liver function, often leading to complications like portal hypertension and liver failure. Fibrosis, being an earlier and potentially reversible accumulation of scar tissue, has a more favorable prognosis if the underlying cause is effectively managed. Long-term outcomes significantly differ, with cirrhosis patients facing higher risks of hepatocellular carcinoma and decreased survival rates compared to those with fibrosis.
Cirrhosis Infographic
 libterm.com
libterm.com