Airway remodeling refers to structural changes in the bronchial walls caused by chronic inflammation, often seen in conditions like asthma and chronic obstructive pulmonary disease (COPD). These changes include thickening of airway walls, increased mucus production, and fibrosis, leading to airflow obstruction and reduced lung function. Discover how understanding airway remodeling can help you manage respiratory diseases more effectively by reading further.
Table of Comparison
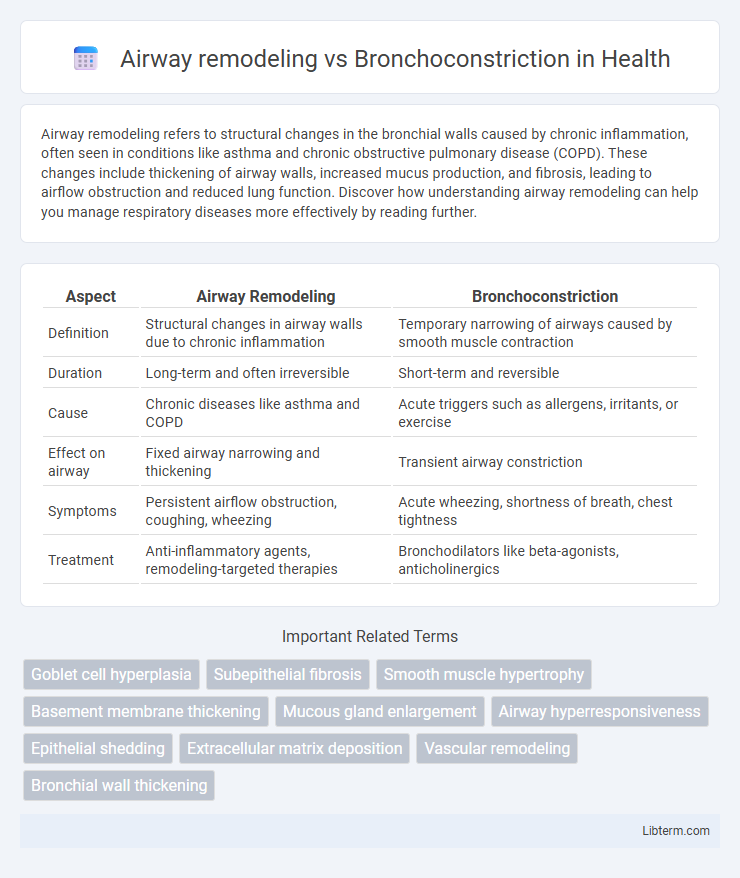
| Aspect | Airway Remodeling | Bronchoconstriction |
|---|---|---|
| Definition | Structural changes in airway walls due to chronic inflammation | Temporary narrowing of airways caused by smooth muscle contraction |
| Duration | Long-term and often irreversible | Short-term and reversible |
| Cause | Chronic diseases like asthma and COPD | Acute triggers such as allergens, irritants, or exercise |
| Effect on airway | Fixed airway narrowing and thickening | Transient airway constriction |
| Symptoms | Persistent airflow obstruction, coughing, wheezing | Acute wheezing, shortness of breath, chest tightness |
| Treatment | Anti-inflammatory agents, remodeling-targeted therapies | Bronchodilators like beta-agonists, anticholinergics |
Introduction to Airway Remodeling and Bronchoconstriction
Airway remodeling involves structural changes in the bronchial walls, including thickening of the airway smooth muscle, increased fibrosis, and goblet cell hyperplasia, which contribute to chronic airflow obstruction in diseases like asthma and chronic obstructive pulmonary disease (COPD). Bronchoconstriction refers to the acute narrowing of the airways caused by contraction of the smooth muscle, leading to reversible airflow limitation and symptoms such as wheezing and shortness of breath. While bronchoconstriction is a functional and often transient response to triggers like allergens or irritants, airway remodeling represents long-term pathological alterations that exacerbate airway hyperresponsiveness and reduce treatment efficacy.
Structural Changes in Airway Remodeling
Airway remodeling involves persistent structural changes such as subepithelial fibrosis, increased smooth muscle mass, and gland hypertrophy that thicken the airway walls and reduce lumen size. These alterations contrast with bronchoconstriction, which is a reversible narrowing of the airways caused by smooth muscle contraction. Understanding remodeling is crucial for addressing chronic respiratory diseases like asthma and COPD where structural changes lead to fixed airflow limitation.
Mechanisms of Bronchoconstriction
Bronchoconstriction primarily involves the contraction of airway smooth muscle triggered by stimuli such as allergens, exercise, or irritants, leading to narrowed bronchial tubes and airflow limitation. This process is mediated by the release of inflammatory mediators like histamine, leukotrienes, and acetylcholine, which activate parasympathetic pathways and induce muscle contraction. Unlike airway remodeling, which involves structural changes including fibrosis and increased smooth muscle mass, bronchoconstriction is a reversible, acute physiological response critical in asthma exacerbations.
Key Differences: Remodeling vs Bronchoconstriction
Airway remodeling involves structural changes in the bronchial walls, such as thickening of the airway smooth muscle and increased extracellular matrix deposition, which contribute to permanent airflow limitation in chronic respiratory diseases. Bronchoconstriction refers to the reversible narrowing of the airways due to contraction of bronchial smooth muscles, leading to acute airflow obstruction typical in asthma attacks. Unlike bronchoconstriction, airway remodeling results in long-term changes that decrease airway elasticity and responsiveness to treatment.
Cellular Pathways Involved
Airway remodeling involves structural changes in the airway wall driven by chronic inflammation, primarily mediated through transforming growth factor-beta (TGF-b) signaling and activation of fibroblasts leading to extracellular matrix deposition. Bronchoconstriction is characterized by acute smooth muscle contraction regulated by G-protein coupled receptor (GPCR) pathways, including the activation of phospholipase C (PLC), increased intracellular calcium, and myosin light chain kinase (MLCK) phosphorylation. Both processes involve complex interactions between cytokines, growth factors, and intracellular signaling cascades but differ in temporal dynamics and cellular targets.
Clinical Manifestations and Symptoms
Airway remodeling leads to persistent airflow limitation characterized by thickened airway walls, increased smooth muscle mass, and fibrosis, resulting in chronic symptoms such as fixed wheezing, dyspnea, and reduced lung function. Bronchoconstriction causes acute, reversible airway narrowing due to smooth muscle contraction, presenting clinically with episodic wheezing, chest tightness, cough, and shortness of breath, often triggered by allergens or irritants. Distinguishing these conditions is critical as remodeling indicates long-term structural changes, whereas bronchoconstriction reflects transient airway hyperresponsiveness.
Diagnostic Approaches
Diagnostic approaches for airway remodeling often include high-resolution computed tomography (HRCT) and pulmonary function tests (PFTs) such as spirometry to assess structural changes and airflow obstruction over time. Bronchoconstriction is primarily evaluated using methacholine challenge tests and peak expiratory flow measurements to detect reversible airway narrowing. Biomarkers in exhaled breath condensate and induced sputum analysis can complement both diagnostics by providing insights into underlying inflammation and tissue remodeling.
Impact on Lung Function
Airway remodeling involves structural changes in the bronchial walls, such as thickening and fibrosis, leading to a persistent decrease in lung function and reduced airway elasticity. Bronchoconstriction causes temporary narrowing of the airways due to smooth muscle contraction, resulting in reversible airflow obstruction and transient breathing difficulties. The chronic nature of airway remodeling results in long-term impairment of airflow, whereas bronchoconstriction primarily affects lung function during acute episodes.
Treatment Strategies and Interventions
Airway remodeling involves structural changes in the bronchial walls, requiring treatment strategies centered on long-term anti-inflammatory therapies such as inhaled corticosteroids and biologics targeting specific inflammatory pathways to prevent irreversible damage. Bronchoconstriction, characterized by acute narrowing of the airways, responds effectively to short-acting bronchodilators like beta-agonists and anticholinergics that provide rapid relief by relaxing airway smooth muscle. Combining both approaches with patient-specific interventions, including pulmonary rehabilitation and adherence to medication regimens, optimizes management of chronic respiratory conditions like asthma and COPD.
Long-term Outcomes and Prognosis
Airway remodeling involves persistent structural changes in the bronchial walls, such as thickening of the basement membrane and increased smooth muscle mass, leading to irreversible airflow limitation and a decline in lung function over time. Bronchoconstriction represents the acute narrowing of airways due to smooth muscle contraction, which is typically reversible with bronchodilator treatment and does not cause permanent tissue damage. Long-term outcomes linked to airway remodeling include chronic respiratory symptoms, progressive airway obstruction, and increased risk of severe asthma exacerbations, while bronchoconstriction primarily contributes to episodic symptoms with a generally favorable prognosis if properly managed.
Airway remodeling Infographic
 libterm.com
libterm.com