Endocarditis is a serious infection of the heart's inner lining, often caused by bacteria entering the bloodstream and attaching to damaged heart valves. Symptoms include fever, fatigue, and heart murmurs, requiring prompt medical diagnosis and treatment to prevent severe complications. Discover more about risk factors, symptoms, and treatment options to protect your heart health in the rest of this article.
Table of Comparison
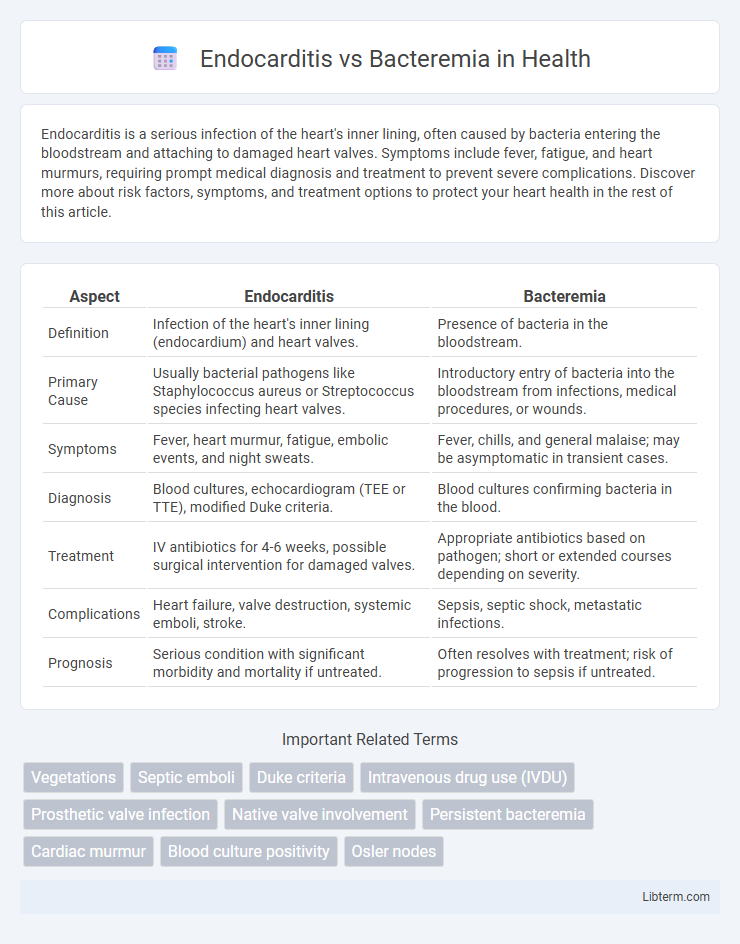
| Aspect | Endocarditis | Bacteremia |
|---|---|---|
| Definition | Infection of the heart's inner lining (endocardium) and heart valves. | Presence of bacteria in the bloodstream. |
| Primary Cause | Usually bacterial pathogens like Staphylococcus aureus or Streptococcus species infecting heart valves. | Introductory entry of bacteria into the bloodstream from infections, medical procedures, or wounds. |
| Symptoms | Fever, heart murmur, fatigue, embolic events, and night sweats. | Fever, chills, and general malaise; may be asymptomatic in transient cases. |
| Diagnosis | Blood cultures, echocardiogram (TEE or TTE), modified Duke criteria. | Blood cultures confirming bacteria in the blood. |
| Treatment | IV antibiotics for 4-6 weeks, possible surgical intervention for damaged valves. | Appropriate antibiotics based on pathogen; short or extended courses depending on severity. |
| Complications | Heart failure, valve destruction, systemic emboli, stroke. | Sepsis, septic shock, metastatic infections. |
| Prognosis | Serious condition with significant morbidity and mortality if untreated. | Often resolves with treatment; risk of progression to sepsis if untreated. |
Introduction to Endocarditis and Bacteremia
Endocarditis is an infection of the inner lining of the heart chambers and valves, primarily caused by bacteria entering the bloodstream and adhering to damaged heart tissue. Bacteremia refers to the presence of bacteria in the bloodstream, which can occur transiently during daily activities or as a result of infections and medical procedures. While bacteremia can be asymptomatic, persistent bacteremia can lead to complications such as endocarditis, making early detection and treatment crucial.
Definition and Overview
Endocarditis is an infection of the inner lining of the heart chambers and valves caused by bacteria, fungi, or other microorganisms, leading to inflammation and potential heart damage. Bacteremia refers to the presence of bacteria in the bloodstream, which may be transient or persistent and can result from infections, medical procedures, or invasive devices. While bacteremia can cause systemic symptoms and may lead to serious complications, endocarditis is a severe localized infection often requiring prolonged antibiotic treatment and sometimes surgery.
Etiology: Causes and Risk Factors
Endocarditis primarily results from bacterial infections such as Staphylococcus aureus and Streptococcus viridans entering the bloodstream and adhering to damaged heart valves or endocardial surfaces. Bacteremia, characterized by the presence of bacteria in the blood, can arise from infections like urinary tract infections, dental procedures, or intravenous catheter use, with common pathogens including Escherichia coli and coagulase-negative staphylococci. Risk factors for endocarditis include pre-existing heart conditions, prosthetic heart valves, and intravenous drug use, while bacteremia risk factors encompass immunosuppression, invasive medical devices, and breaches in skin or mucosal barriers.
Pathophysiology: Disease Mechanisms
Endocarditis involves infection and inflammation of the heart's inner lining, primarily caused by bacterial colonization on damaged heart valves, leading to vegetation formation and potential embolic events. Bacteremia refers to the presence of bacteria in the bloodstream, which can be transient or persistent and may result from infections, invasive procedures, or immune compromise, potentially seeding distant sites including heart valves. The pathophysiology of endocarditis is closely linked to bacteremia, where circulating bacteria adhere to endothelial surfaces, initiating an inflammatory cascade critical to disease progression.
Clinical Presentation: Signs and Symptoms
Endocarditis typically presents with persistent fever, new or changing heart murmurs, and signs of embolic phenomena such as petechiae or Janeway lesions. Bacteremia often manifests as transient fever, chills, and chills without localized findings, though it can progress to sepsis if untreated. Both conditions may share nonspecific symptoms like fatigue and malaise, but the presence of cardiac-specific signs distinguishes endocarditis clinically.
Diagnostic Approach: Tests and Criteria
Diagnosis of endocarditis primarily relies on the Modified Duke Criteria, incorporating clinical, microbiological, and echocardiographic findings. Blood cultures are essential in both endocarditis and bacteremia diagnosis to identify causative pathogens, but echocardiography--especially transesophageal echocardiography (TEE)--is critical for detecting vegetations or cardiac complications in endocarditis. Laboratory tests such as inflammatory markers (CRP, ESR) support diagnosis but lack specificity, making combined clinical assessment and imaging decisive for differentiating endocarditis from uncomplicated bacteremia.
Treatment Strategies and Management
Treatment strategies for endocarditis involve prolonged intravenous antibiotic therapy tailored to the specific causative organism, with surgical intervention considered for complications such as valve destruction or persistent infection. Bacteremia typically requires targeted antimicrobial therapy based on blood culture results, with duration varying depending on whether the infection is uncomplicated or linked to an indwelling device or a focus of infection. Management of endocarditis demands close monitoring through echocardiography and inflammatory markers, whereas bacteremia management emphasizes source control and prevention of progression to endocarditis or sepsis.
Complications and Prognosis
Endocarditis commonly leads to severe complications such as valvular damage, heart failure, and embolic events including stroke, which significantly worsen long-term prognosis. Bacteremia, while potentially transient, can progress to sepsis or seed distant infections, raising morbidity risk if not promptly managed. Early diagnosis and targeted antibiotic therapy improve outcomes for both conditions, but infective endocarditis carries a higher mortality rate compared to uncomplicated bacteremia.
Prevention and Risk Reduction
Preventing endocarditis and bacteremia involves meticulous oral hygiene and timely treatment of infections to reduce bacterial entry into the bloodstream. High-risk individuals, such as those with prosthetic heart valves or previous endocarditis, should receive prophylactic antibiotics before invasive dental or surgical procedures to lower infection risk. Maintaining a strong immune system and promptly addressing intravenous drug use can further minimize the chances of bacteremia progressing to serious complications like endocarditis.
Key Differences: Endocarditis vs Bacteremia
Endocarditis is an infection of the heart's inner lining, particularly affecting the heart valves, caused by bacteria or fungi that form vegetations, whereas bacteremia refers to the presence of bacteria in the bloodstream without necessarily causing infection. Endocarditis symptoms include fever, heart murmur, and embolic events, requiring prolonged antibiotic therapy and sometimes surgery, while bacteremia can be transient or persistent, often detected through blood cultures and treated according to the source. The key difference lies in endocarditis causing a localized, severe infection of heart tissue with potential complications, whereas bacteremia is a systemic condition that may be asymptomatic or lead to sepsis if untreated.
Endocarditis Infographic
 libterm.com
libterm.com