Fungemia is a serious bloodstream infection caused by fungi, often Candida species, entering the bloodstream and spreading throughout the body. Prompt diagnosis and treatment are critical to prevent complications such as organ failure or sepsis. Explore the rest of this article to learn about the symptoms, risk factors, and effective treatments for fungemia to protect your health.
Table of Comparison
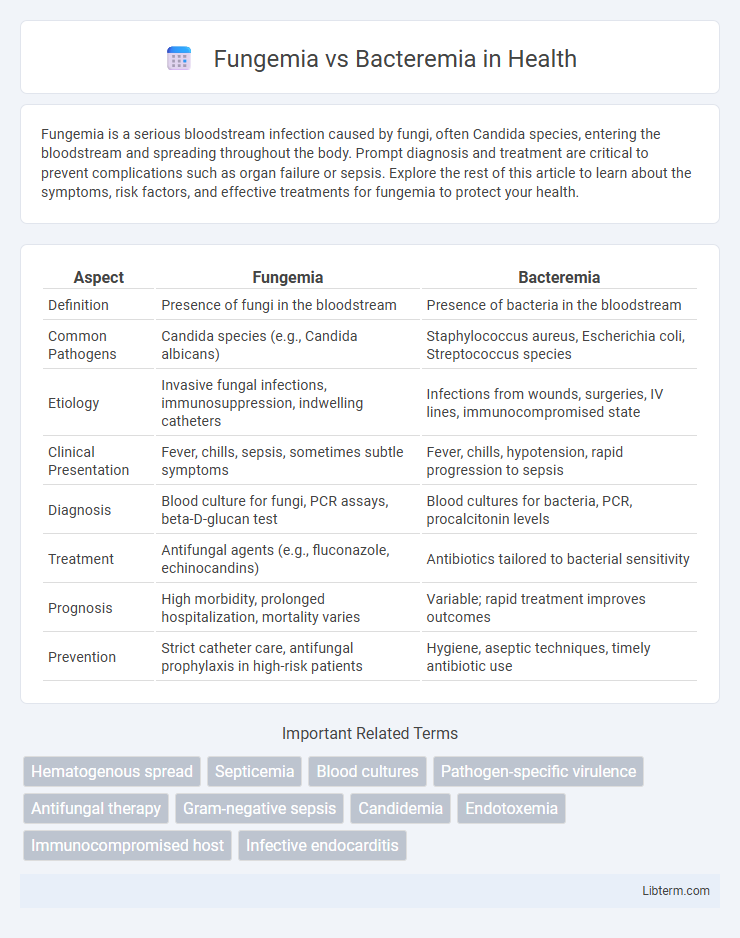
| Aspect | Fungemia | Bacteremia |
|---|---|---|
| Definition | Presence of fungi in the bloodstream | Presence of bacteria in the bloodstream |
| Common Pathogens | Candida species (e.g., Candida albicans) | Staphylococcus aureus, Escherichia coli, Streptococcus species |
| Etiology | Invasive fungal infections, immunosuppression, indwelling catheters | Infections from wounds, surgeries, IV lines, immunocompromised state |
| Clinical Presentation | Fever, chills, sepsis, sometimes subtle symptoms | Fever, chills, hypotension, rapid progression to sepsis |
| Diagnosis | Blood culture for fungi, PCR assays, beta-D-glucan test | Blood cultures for bacteria, PCR, procalcitonin levels |
| Treatment | Antifungal agents (e.g., fluconazole, echinocandins) | Antibiotics tailored to bacterial sensitivity |
| Prognosis | High morbidity, prolonged hospitalization, mortality varies | Variable; rapid treatment improves outcomes |
| Prevention | Strict catheter care, antifungal prophylaxis in high-risk patients | Hygiene, aseptic techniques, timely antibiotic use |
Introduction to Fungemia and Bacteremia
Fungemia and bacteremia both refer to the presence of microorganisms in the bloodstream, with fungemia involving fungal pathogens such as Candida species and bacteremia involving bacterial agents like Staphylococcus aureus or Escherichia coli. These bloodstream infections pose significant risks, often leading to systemic inflammatory response syndrome (SIRS) or sepsis if untreated, and require prompt identification through blood cultures and targeted antimicrobial therapy. Understanding the distinct etiologies and clinical implications of fungemia versus bacteremia is critical for effective diagnosis and treatment in immunocompromised patients and those with indwelling medical devices.
Definition and Key Differences
Fungemia refers to the presence of fungi, particularly Candida species, in the bloodstream, often leading to systemic fungal infections, whereas bacteremia involves the presence of bacteria such as Staphylococcus aureus or Escherichia coli in the blood. Fungemia is typically associated with immunocompromised patients and may require antifungal treatment, while bacteremia can result from various infections and commonly necessitates antibiotic therapy. Key differences include the causative microorganisms, clinical risk factors, diagnostic methods like blood cultures, and targeted treatment protocols.
Common Causes and Risk Factors
Fungemia is primarily caused by Candida species, especially Candida albicans, and is often associated with immunocompromised individuals, indwelling catheters, and prolonged antibiotic use. Bacteremia commonly results from Staphylococcus aureus, Escherichia coli, and Streptococcus species, with risk factors including invasive procedures, chronic illnesses like diabetes, and breaches in skin integrity. Both conditions share risk factors such as hospitalization, immunosuppression, and the presence of foreign medical devices.
Pathophysiology: How Infections Develop
Fungemia occurs when fungal pathogens, primarily Candida species, enter the bloodstream and evade the immune system by forming biofilms and hyphal structures, leading to systemic infection. Bacteremia involves the presence of bacteria such as Staphylococcus aureus or Escherichia coli in the blood, often resulting from local infections or invasive procedures that disrupt mucosal barriers. Both conditions trigger immune responses, but fungi tend to persist longer due to their complex cell wall structures and ability to resist phagocytosis, influencing the severity and progression of infection.
Clinical Manifestations and Symptoms
Fungemia typically presents with fever, chills, and symptoms of sepsis, often accompanied by hypotension and multi-organ dysfunction in severe cases, especially in immunocompromised patients. Bacteremia manifests with fever, chills, tachycardia, and may progress to septic shock or localized infections depending on the bacterial strain and patient immune status. Both conditions can cause systemic inflammatory response syndrome (SIRS), but fungemia often has a more insidious onset and is associated with prolonged hospital stays and indwelling catheters.
Diagnostic Approaches and Testing
Diagnostic approaches for fungemia rely on blood cultures using fungal-specific media and molecular methods such as PCR to detect fungal DNA, providing faster and more sensitive identification compared to traditional culture techniques. Bacteremia diagnosis primarily involves standard blood cultures with aerobic and anaerobic bottles, complemented by rapid molecular assays like multiplex PCR panels to detect bacterial pathogens and resistance genes. Both conditions benefit from antigen detection tests and next-generation sequencing in complex or culture-negative cases, enhancing diagnostic accuracy and guiding targeted antimicrobial or antifungal therapy.
Treatment Strategies and Options
Treatment strategies for fungemia primarily involve antifungal agents such as echinocandins, azoles, or amphotericin B, depending on the fungal species and patient-specific factors, whereas bacteremia is managed with targeted antibacterial therapy guided by culture and sensitivity results. Central venous catheter removal is critical in both conditions to reduce pathogen burden and improve outcomes. Supportive care, including hemodynamic stabilization and monitoring for organ dysfunction, complements antimicrobial treatment in severe cases of fungemia and bacteremia.
Complications and Prognosis
Fungemia often leads to severe complications such as endocarditis, disseminated infections, and organ failure, with a generally higher mortality rate compared to bacteremia. Bacteremia commonly causes sepsis, septic shock, and metastatic infections, but its prognosis improves significantly with early antibiotic treatment. Both conditions require prompt diagnosis and targeted therapy to reduce morbidity and prevent long-term complications.
Prevention and Infection Control
Preventing fungemia and bacteremia requires stringent infection control practices, including proper hand hygiene, sterilization of medical equipment, and timely removal of invasive devices like catheters to reduce the risk of bloodstream infections. Use of antifungal prophylaxis in high-risk patients, such as those with immunosuppression, and strict antimicrobial stewardship programs minimize the development and spread of resistant fungal and bacterial strains. Isolation protocols and environmental cleaning further control nosocomial infections, limiting the incidence of both fungemia caused by Candida species and bacteremia primarily due to Staphylococcus aureus or Gram-negative bacteria.
Summary and Future Perspectives
Fungemia and bacteremia represent bloodstream infections caused by fungi and bacteria, respectively, both posing significant clinical challenges with varying pathogen profiles and treatment protocols. Advances in rapid diagnostic techniques and targeted antifungal and antibacterial therapies offer promising avenues to improve patient outcomes and reduce mortality rates. Future research is expected to focus on developing precise biomarkers, personalized medicine approaches, and enhanced antimicrobial stewardship to combat resistance and optimize therapeutic strategies.
Fungemia Infographic
 libterm.com
libterm.com