Ejection refers to the forceful expulsion of an object or substance from a container or system, often observed in various scientific and medical contexts. Understanding the mechanisms behind ejection can enhance your knowledge of processes ranging from cardiac function to aerospace propulsion. Continue reading to explore the detailed principles and applications of ejection.
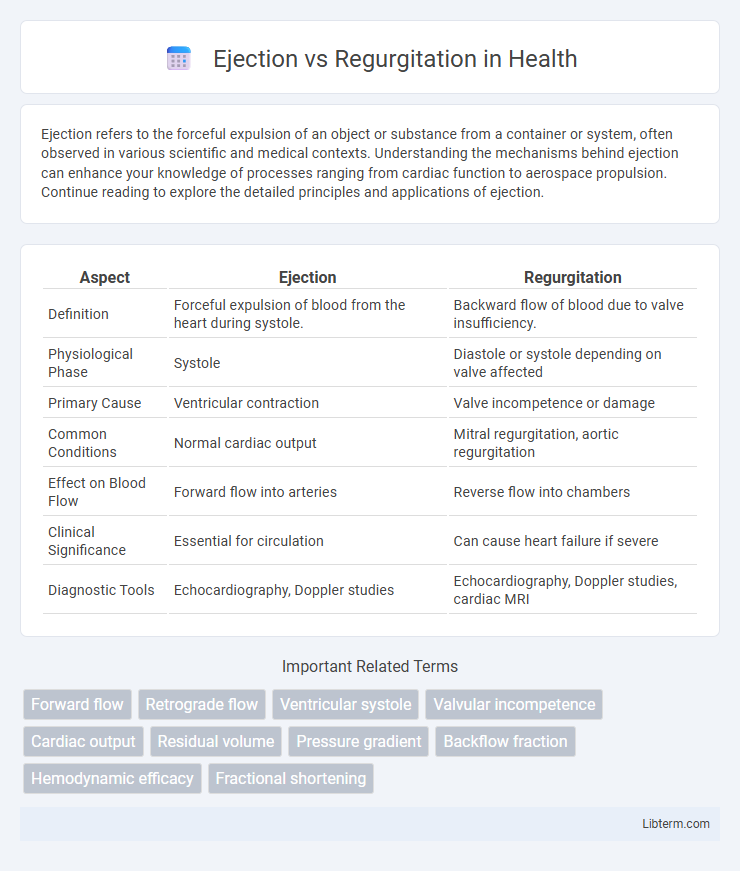
Table of Comparison
| Aspect | Ejection | Regurgitation |
|---|---|---|
| Definition | Forceful expulsion of blood from the heart during systole. | Backward flow of blood due to valve insufficiency. |
| Physiological Phase | Systole | Diastole or systole depending on valve affected |
| Primary Cause | Ventricular contraction | Valve incompetence or damage |
| Common Conditions | Normal cardiac output | Mitral regurgitation, aortic regurgitation |
| Effect on Blood Flow | Forward flow into arteries | Reverse flow into chambers |
| Clinical Significance | Essential for circulation | Can cause heart failure if severe |
| Diagnostic Tools | Echocardiography, Doppler studies | Echocardiography, Doppler studies, cardiac MRI |
Introduction to Ejection and Regurgitation
Ejection and regurgitation are two distinct cardiac valve dysfunctions characterized by abnormal blood flow patterns within the heart. Ejection refers to the forward flow of blood from the ventricles into the arteries during systole, while regurgitation involves the backward leakage of blood through a valve that fails to close properly during diastole or systole. Understanding the hemodynamic impact of ejection and regurgitation is critical for diagnosing valvular heart diseases such as aortic stenosis and mitral regurgitation.
Defining Ejection in Cardiac Physiology
Ejection in cardiac physiology refers to the process during systole when the heart's ventricles contract to propel blood through the semilunar valves into the aorta and pulmonary artery. This phase is critical for maintaining effective cardiac output and ensuring oxygenated blood reaches systemic circulation. Ejection fraction, a key clinical parameter, quantifies the percentage of blood ejected from the ventricle with each heartbeat, providing insight into ventricular function.
Understanding Regurgitation in Heart Valves
Regurgitation in heart valves occurs when the valve fails to close properly, causing blood to flow backward into the heart chamber. This condition leads to volume overload, reduced cardiac efficiency, and can eventually cause heart enlargement or failure if untreated. Differentiating regurgitation from ejection abnormalities is critical for targeted treatment and accurate diagnosis using echocardiography and Doppler studies.
Key Differences Between Ejection and Regurgitation
Ejection refers to the forceful expulsion of blood from the heart's ventricles during systole, while regurgitation denotes the backward flow of blood due to valve incompetence. Ejection is characterized by forward stroke volume and efficient cardiac output, whereas regurgitation leads to volume overload and reduced hemodynamic efficiency. Key diagnostic differences include systolic murmur intensity in ejection versus abnormal backward flow detected via Doppler echocardiography in regurgitation.
Causes of Impaired Cardiac Ejection
Impaired cardiac ejection commonly results from systolic dysfunction caused by ischemic heart disease, which reduces myocardial contractility and stroke volume. Other significant causes include cardiomyopathies, such as dilated cardiomyopathy, leading to weakened ventricular walls and decreased ejection fraction. Valvular abnormalities like aortic stenosis increase afterload, further compromising cardiac output by impairing effective ejection during systole.
Common Factors Leading to Regurgitation
Common factors leading to regurgitation include valve abnormalities such as mitral valve prolapse or aortic insufficiency, which cause improper closure and allow blood to flow backward. Structural damage from infections like endocarditis or rheumatic heart disease can also impair valve function, contributing to regurgitation. Furthermore, conditions causing left ventricular dilation or papillary muscle dysfunction often exacerbate valve incompetence and promote regurgitant flow.
Diagnostic Tools for Ejection vs Regurgitation
Echocardiography remains the primary diagnostic tool for differentiating ejection from regurgitation, providing detailed assessment of valve structure, flow patterns, and ventricular function. Doppler ultrasound quantifies blood flow velocity and direction, helping to distinguish between forward ejection and backward regurgitant flow. Cardiac MRI offers complementary data on ventricular volume and myocardial damage, improving diagnostic accuracy in complex cases of valvular dysfunction.
Effects of Ejection and Regurgitation on Heart Function
Ejection refers to the forceful expulsion of blood from the ventricles during systole, which maintains efficient cardiac output and systemic circulation. Regurgitation involves the backward flow of blood through incompetent valves, leading to volume overload, increased ventricular workload, and potential heart failure. Both altered ejection and valve regurgitation disrupt normal hemodynamics, impair myocardial function, and can contribute to progressive cardiac remodeling.
Treatments for Ejection Abnormalities and Regurgitation
Treatment for ejection abnormalities primarily involves medications such as beta-blockers, ACE inhibitors, and calcium channel blockers to improve cardiac output and reduce afterload, while severe cases may require surgical interventions like valve repair or replacement. Regurgitation management depends on the severity and cause, where mild cases are monitored with regular echocardiograms and lifestyle modifications, and more severe regurgitation often necessitates surgical repair or valve replacement to prevent heart failure. Percutaneous techniques such as transcatheter valve repair or replacement have emerged as minimally invasive options for patients at high surgical risk.
Prognosis and Long-Term Outcomes
Ejection fraction reduction in ejection disorders often correlates with a worse prognosis, including increased risk of heart failure and mortality, especially in cases of systolic dysfunction. In contrast, regurgitation disorders may preserve ejection fraction but lead to volume overload, progressive ventricular dilation, and eventual heart failure if left untreated. Long-term outcomes improve significantly with timely surgical intervention or medical management tailored to mitigate ventricular remodeling and preserve cardiac function.
Ejection Infographic
 libterm.com
libterm.com