Cholecystitis is the inflammation of the gallbladder, often caused by gallstones blocking the bile ducts, leading to severe abdominal pain and digestive issues. Pancreatitis involves inflammation of the pancreas, which can result from gallstones or excessive alcohol consumption, causing intense abdominal pain and digestive enzyme disruption. Discover how these conditions are diagnosed, treated, and what steps you can take to manage your health by reading the rest of the article.
Table of Comparison
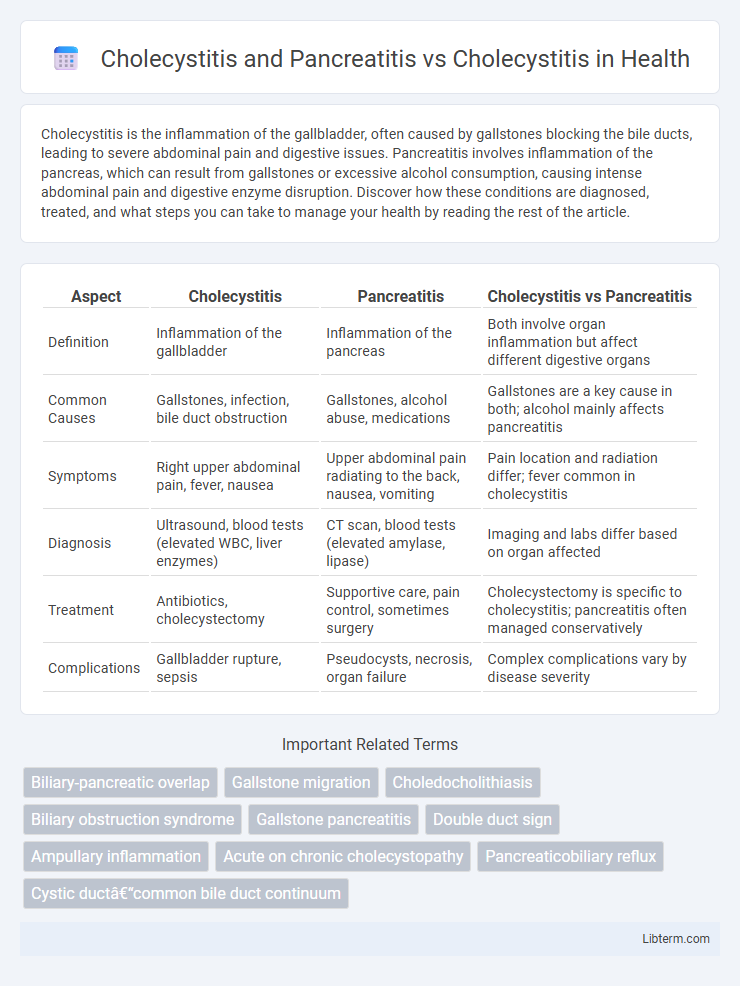
| Aspect | Cholecystitis | Pancreatitis | Cholecystitis vs Pancreatitis |
|---|---|---|---|
| Definition | Inflammation of the gallbladder | Inflammation of the pancreas | Both involve organ inflammation but affect different digestive organs |
| Common Causes | Gallstones, infection, bile duct obstruction | Gallstones, alcohol abuse, medications | Gallstones are a key cause in both; alcohol mainly affects pancreatitis |
| Symptoms | Right upper abdominal pain, fever, nausea | Upper abdominal pain radiating to the back, nausea, vomiting | Pain location and radiation differ; fever common in cholecystitis |
| Diagnosis | Ultrasound, blood tests (elevated WBC, liver enzymes) | CT scan, blood tests (elevated amylase, lipase) | Imaging and labs differ based on organ affected |
| Treatment | Antibiotics, cholecystectomy | Supportive care, pain control, sometimes surgery | Cholecystectomy is specific to cholecystitis; pancreatitis often managed conservatively |
| Complications | Gallbladder rupture, sepsis | Pseudocysts, necrosis, organ failure | Complex complications vary by disease severity |
Overview of Cholecystitis and Pancreatitis
Cholecystitis is the inflammation of the gallbladder, often caused by gallstones blocking the cystic duct, resulting in severe abdominal pain and potential infection. Pancreatitis refers to inflammation of the pancreas, commonly triggered by gallstones or excessive alcohol consumption, leading to enzymatic digestion of pancreatic tissue and systemic complications. Both conditions share overlapping symptoms like abdominal pain and digestive disturbances but differ in their organ-specific pathology and treatment approaches.
Key Differences Between Cholecystitis and Cholecystitis With Pancreatitis
Cholecystitis involves inflammation of the gallbladder typically caused by gallstones, leading to localized right upper quadrant pain and fever. Cholecystitis with pancreatitis presents a more complex clinical picture with simultaneous inflammation of the pancreas, often resulting from gallstone migration obstructing the pancreatic duct, causing severe abdominal pain, elevated pancreatic enzymes, and systemic inflammatory response. The key difference lies in the involvement of the pancreas and the severity of symptoms, with pancreatitis complicating cholecystitis by increasing risks of necrosis, infection, and multi-organ dysfunction.
Etiology: Causes of Cholecystitis vs Combined Conditions
Cholecystitis primarily results from gallstone obstruction of the cystic duct leading to inflammation, with risk factors including gallstones, infection, and bile stasis. When cholecystitis occurs with pancreatitis, the underlying cause often involves shared etiologies such as gallstone migration causing blockage at the ampulla of Vater, triggering both gallbladder inflammation and pancreatic enzyme activation. The combined condition reflects a more complex pathophysiology driven by gallstone-induced biliary obstruction and subsequent pancreatic injury.
Pathophysiology: Disease Mechanisms Compared
Cholecystitis primarily involves inflammation of the gallbladder due to cystic duct obstruction, often caused by gallstones, leading to bile stasis and subsequent infection or ischemia. Pancreatitis, in contrast, results from premature activation of pancreatic enzymes causing autodigestion of pancreatic tissue, frequently triggered by gallstone migration or alcohol abuse. While both conditions involve biliary pathology, cholecystitis centers on localized gallbladder inflammation, whereas pancreatitis involves systemic inflammatory response due to pancreatic tissue injury.
Clinical Presentation: Symptoms Contrast
Cholecystitis typically presents with right upper quadrant abdominal pain, fever, and nausea, often triggered by gallstone obstruction. Pancreatitis symptoms include severe epigastric pain radiating to the back, accompanied by nausea, vomiting, and elevated pancreatic enzymes. Unlike isolated cholecystitis, pancreatitis often causes systemic inflammatory response and more intense abdominal tenderness.
Diagnostic Approaches: Cholecystitis Alone vs With Pancreatitis
Diagnostic approaches for cholecystitis alone primarily involve abdominal ultrasound, which effectively identifies gallbladder wall thickening, stones, and pericholecystic fluid. When pancreatitis coexists with cholecystitis, diagnostic protocols expand to include serum lipase and amylase levels, alongside enhanced imaging techniques such as contrast-enhanced CT scans or MRCP to evaluate pancreatic inflammation and ductal obstructions. Combining biochemical markers with advanced imaging improves accuracy in distinguishing between isolated cholecystitis and concurrent pancreatitis, guiding targeted therapeutic interventions.
Laboratory and Imaging Findings
Cholecystitis typically presents with elevated white blood cell count and mild increases in liver enzymes, with ultrasound revealing gallbladder wall thickening, pericholecystic fluid, and gallstones. In cases of cholecystitis combined with pancreatitis, laboratory findings include significantly elevated serum amylase and lipase levels, alongside abnormalities in liver function tests indicating biliary obstruction. Imaging modalities such as abdominal ultrasound or CT scan demonstrate inflammation of both the gallbladder and pancreas, with possible pancreatic edema or necrosis in pancreatitis cases.
Treatment Strategies: Similarities and Differences
Treatment strategies for cholecystitis and pancreatitis overlap in initial management, including pain control, fluid resuscitation, and fasting to rest the digestive system. Cholecystitis often requires antibiotics and cholecystectomy, whereas pancreatitis treatment focuses on addressing underlying causes like gallstones or alcohol use, with surgical intervention reserved for severe cases or complications. Both conditions benefit from supportive care and monitoring, but the timing and specific interventions diverge based on disease severity and organ involvement.
Prognosis and Complications
Cholecystitis combined with pancreatitis generally presents a more severe prognosis due to the involvement of both the gallbladder and pancreas, increasing the risk of systemic inflammation and multi-organ dysfunction. Common complications include pancreatic necrosis, abscess formation, and prolonged hospital stay compared to isolated cholecystitis, which primarily risks gallbladder empyema or perforation. Early diagnosis and management are crucial to reduce morbidity and improve outcomes in cases where both conditions coexist.
Prevention and Patient Education
Prevention of cholecystitis and pancreatitis involves maintaining a healthy diet rich in fiber and low in saturated fats to reduce gallstone formation, the primary cause of cholecystitis and pancreatitis. Patient education emphasizes recognizing early symptoms such as severe abdominal pain and seeking prompt medical attention to prevent complications like gallbladder infection or pancreatic inflammation. Regular monitoring for high-risk individuals, including those with obesity, diabetes, or a history of gallstones, supports early intervention and improved outcomes in managing these conditions.
Cholecystitis and Pancreatitis Infographic
 libterm.com
libterm.com