Cellulitis is a common bacterial skin infection characterized by redness, swelling, warmth, and pain. Prompt treatment with antibiotics is crucial to prevent the infection from spreading and causing serious complications. Learn more about the causes, symptoms, and effective treatments to protect your health in the rest of this article.
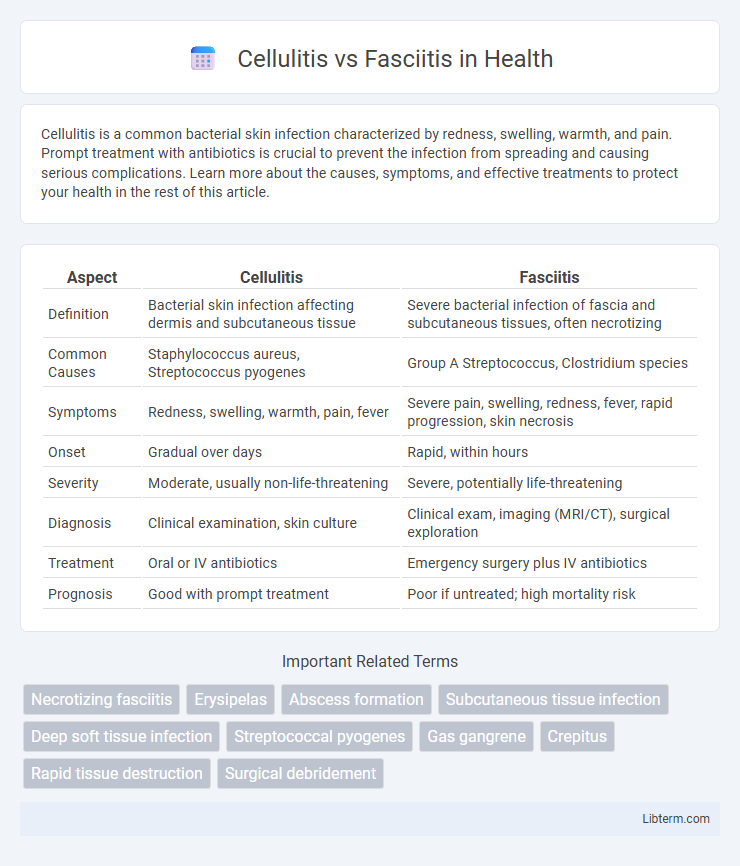
Table of Comparison
| Aspect | Cellulitis | Fasciitis |
|---|---|---|
| Definition | Bacterial skin infection affecting dermis and subcutaneous tissue | Severe bacterial infection of fascia and subcutaneous tissues, often necrotizing |
| Common Causes | Staphylococcus aureus, Streptococcus pyogenes | Group A Streptococcus, Clostridium species |
| Symptoms | Redness, swelling, warmth, pain, fever | Severe pain, swelling, redness, fever, rapid progression, skin necrosis |
| Onset | Gradual over days | Rapid, within hours |
| Severity | Moderate, usually non-life-threatening | Severe, potentially life-threatening |
| Diagnosis | Clinical examination, skin culture | Clinical exam, imaging (MRI/CT), surgical exploration |
| Treatment | Oral or IV antibiotics | Emergency surgery plus IV antibiotics |
| Prognosis | Good with prompt treatment | Poor if untreated; high mortality risk |
Understanding Cellulitis and Fasciitis
Cellulitis is a bacterial skin infection characterized by redness, swelling, warmth, and pain, primarily affecting the dermis and subcutaneous tissues, commonly caused by Streptococcus or Staphylococcus species. Fasciitis, particularly necrotizing fasciitis, is a severe, rapidly progressing infection targeting the fascia, the connective tissue surrounding muscles, often caused by mixed bacterial pathogens including Group A Streptococcus. Differentiating cellulitis from fasciitis involves recognizing the depth of tissue involvement and severity, as fasciitis requires urgent surgical intervention alongside antibiotics to prevent systemic complications and tissue necrosis.
Key Differences Between Cellulitis and Fasciitis
Cellulitis is a superficial bacterial skin infection affecting the dermis and subcutaneous tissues, characterized by redness, warmth, swelling, and pain, commonly caused by Streptococcus or Staphylococcus species. Fasciitis, particularly necrotizing fasciitis, is a rapidly progressing infection involving the fascia and subcutaneous tissues, often caused by Group A Streptococcus or mixed bacterial flora, leading to severe tissue necrosis and systemic toxicity. Early differentiation is critical as cellulitis typically responds to antibiotics alone, while fasciitis often requires urgent surgical intervention to prevent high morbidity and mortality.
Causes and Risk Factors
Cellulitis is caused by bacterial infections, primarily Streptococcus and Staphylococcus species, entering through breaks in the skin, while necrotizing fasciitis involves a more aggressive infection that rapidly destroys fascia and subcutaneous tissue, commonly triggered by Group A Streptococcus and mixed aerobic and anaerobic bacteria. Risk factors for cellulitis include diabetes, immune suppression, chronic skin conditions, and lymphedema, whereas fasciitis risk factors encompass trauma, surgery, immunocompromised states, and intravenous drug use. Both conditions require prompt recognition but fasciitis demands urgent surgical intervention due to its rapid progression and high mortality risk.
Clinical Presentation: Signs and Symptoms
Cellulitis presents with localized skin redness, warmth, swelling, and tenderness, often accompanied by fever and malaise. Necrotizing fasciitis exhibits rapid progression with severe pain disproportionate to skin findings, swelling, erythema, and systemic symptoms like high fever and hypotension. Early recognition of disproportionate pain and systemic toxicity is crucial for differentiating necrotizing fasciitis from cellulitis in clinical practice.
Diagnostic Criteria and Procedures
Cellulitis is diagnosed primarily through clinical examination, characterized by localized redness, warmth, swelling, and tenderness, with laboratory tests such as elevated white blood cell count supporting the diagnosis. Necrotizing fasciitis requires a higher index of suspicion, with diagnostic procedures including imaging modalities like MRI or CT scans revealing fascial edema and gas formation, alongside surgical exploration for definitive identification. Rapid differentiation is critical, as fasciitis presents with severe pain disproportionate to physical findings, systemic toxicity, and requires urgent debridement compared to conservative antibiotic management for cellulitis.
Complications and Severity
Cellulitis primarily affects the skin and subcutaneous tissues, resulting in localized redness, swelling, and pain, but may lead to complications like abscess formation or sepsis if untreated. Necrotizing fasciitis, also known as flesh-eating disease, is a rapidly progressing infection of the fascia and underlying tissues, often causing systemic toxicity, multi-organ failure, and a high mortality rate without prompt surgical intervention. Early differentiation between cellulitis and fasciitis is critical due to the latter's aggressive nature and potential for severe, life-threatening complications.
Treatment and Management Options
Treatment for cellulitis primarily involves oral or intravenous antibiotics targeting common pathogens such as Streptococcus and Staphylococcus species to reduce infection and inflammation. Fasciitis, particularly necrotizing fasciitis, requires aggressive surgical debridement combined with broad-spectrum intravenous antibiotics to halt rapid tissue destruction and sepsis. Supportive care in an intensive care setting, including fluid resuscitation and organ support, is critical for managing severe fasciitis cases.
Preventive Measures and Early Detection
Preventive measures for cellulitis and fasciitis include maintaining proper skin hygiene, promptly treating wounds or insect bites, and managing underlying conditions such as diabetes or immune disorders to reduce infection risk. Early detection relies on recognizing symptoms like redness, swelling, warmth, and severe pain, with fasciitis often presenting rapid progression and systemic signs such as fever or shock. Timely medical evaluation with imaging and laboratory tests is critical to differentiate cellulitis from the more aggressive necrotizing fasciitis and initiate appropriate antibiotic or surgical treatment.
Prognosis and Recovery
Cellulitis, a bacterial skin infection affecting the dermis and subcutaneous tissue, generally has a favorable prognosis with timely antibiotic treatment, leading to full recovery in most cases within 7 to 10 days. Necrotizing fasciitis, a severe soft tissue infection involving the fascia and deeper layers, requires urgent surgical intervention and aggressive antibiotics, with a prognosis heavily dependent on early diagnosis; delayed treatment significantly increases mortality rates, often exceeding 20-30%. Recovery from necrotizing fasciitis involves prolonged wound care, possible reconstructive surgery, and extended rehabilitation, contrasting with the relatively straightforward healing process seen in cellulitis.
When to Seek Immediate Medical Attention
Severe pain, rapid spreading redness, swelling, and fever indicate the need for immediate medical attention in cases of cellulitis and necrotizing fasciitis. Necrotizing fasciitis often presents with intense pain disproportionate to the visible symptoms, requiring emergency intervention to prevent tissue death and sepsis. If symptoms worsen quickly or systemic signs such as confusion, high fever, or low blood pressure develop, urgent hospital care is critical to improve outcomes.
Cellulitis Infographic
 libterm.com
libterm.com