Hypomagnesemia is a condition characterized by abnormally low levels of magnesium in the blood, affecting muscle function, heart rhythm, and nerve signaling. Common causes include chronic alcoholism, certain medications, and gastrointestinal disorders that impair magnesium absorption. Discover how identifying symptoms and managing hypomagnesemia can improve your health by reading the full article.
Table of Comparison
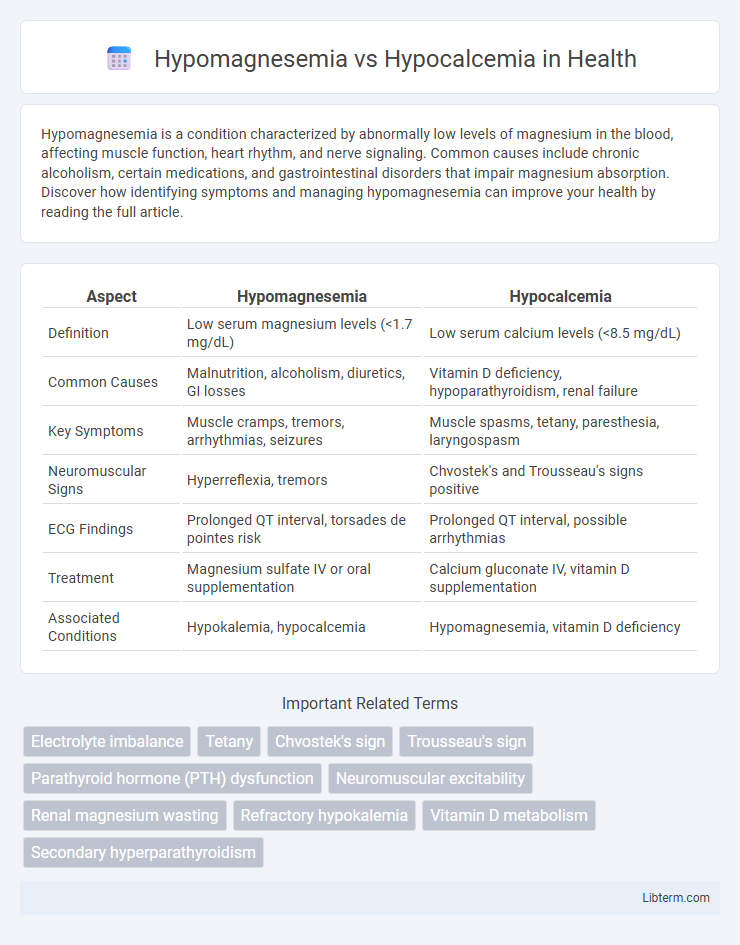
| Aspect | Hypomagnesemia | Hypocalcemia |
|---|---|---|
| Definition | Low serum magnesium levels (<1.7 mg/dL) | Low serum calcium levels (<8.5 mg/dL) |
| Common Causes | Malnutrition, alcoholism, diuretics, GI losses | Vitamin D deficiency, hypoparathyroidism, renal failure |
| Key Symptoms | Muscle cramps, tremors, arrhythmias, seizures | Muscle spasms, tetany, paresthesia, laryngospasm |
| Neuromuscular Signs | Hyperreflexia, tremors | Chvostek's and Trousseau's signs positive |
| ECG Findings | Prolonged QT interval, torsades de pointes risk | Prolonged QT interval, possible arrhythmias |
| Treatment | Magnesium sulfate IV or oral supplementation | Calcium gluconate IV, vitamin D supplementation |
| Associated Conditions | Hypokalemia, hypocalcemia | Hypomagnesemia, vitamin D deficiency |
Introduction to Hypomagnesemia and Hypocalcemia
Hypomagnesemia is a clinical condition characterized by abnormally low magnesium levels in the blood, often defined as serum magnesium below 1.7 mg/dL, impacting numerous enzymatic processes and neuromuscular function. Hypocalcemia refers to a state of low calcium concentration in the bloodstream, typically below 8.5 mg/dL, affecting bone metabolism, muscle contraction, and nerve signaling. Both disorders disrupt mineral homeostasis and may present with overlapping symptoms such as muscle cramps, tetany, and cardiac arrhythmias, necessitating precise laboratory diagnosis for effective management.
Definitions and Key Differences
Hypomagnesemia is a condition characterized by low magnesium levels in the blood, typically below 1.7 mg/dL, affecting neuromuscular and cardiovascular function. Hypocalcemia refers to decreased calcium levels in the blood, generally under 8.5 mg/dL, impacting bone health and muscle contractions. The key difference lies in their mineral deficiencies and primary clinical manifestations: hypomagnesemia often causes muscle cramps and arrhythmias, while hypocalcemia leads to tetany and neurological symptoms.
Causes of Hypomagnesemia
Hypomagnesemia primarily results from inadequate dietary intake, chronic alcoholism, gastrointestinal losses such as diarrhea or malabsorption, and renal magnesium wasting due to diuretics or certain genetic disorders. Unlike hypocalcemia, which often arises from vitamin D deficiency or parathyroid hormone dysfunction, hypomagnesemia directly impairs parathyroid hormone secretion and action, leading to secondary hypocalcemia. Identifying underlying causes like proton pump inhibitor use or uncontrolled diabetes is critical for effective management of hypomagnesemia.
Causes of Hypocalcemia
Hypocalcemia primarily results from vitamin D deficiency, hypoparathyroidism, and chronic kidney disease, which impair calcium absorption or regulation. Other causes include acute pancreatitis, certain medications like bisphosphonates, and magnesium deficiency, which affects parathyroid hormone secretion. Understanding these etiologies is crucial for distinguishing hypocalcemia from hypomagnesemia, since magnesium imbalance can also influence calcium levels.
Clinical Manifestations and Symptoms
Hypomagnesemia commonly presents with neuromuscular irritability, including muscle cramps, tremors, and tetany, often accompanied by seizures and cardiac arrhythmias such as prolonged QT interval. Hypocalcemia manifests with similar neuromuscular symptoms like paresthesias, muscle spasms (notably Chvostek and Trousseau signs), and in severe cases, laryngospasm or seizures. Both electrolyte imbalances can cause fatigue and mental status changes, but hypomagnesemia may also impair parathyroid hormone secretion, exacerbating hypocalcemia symptoms.
Diagnostic Approaches and Laboratory Findings
Hypomagnesemia diagnosis involves measuring serum magnesium levels, often revealing values below 1.7 mg/dL, with associated low ionized magnesium and possible concurrent hypokalemia or hypocalcemia. In hypocalcemia, serum total calcium below 8.5 mg/dL or ionized calcium under 4.5 mg/dL, alongside elevated parathyroid hormone (PTH) in secondary hypocalcemia, indicates the condition. Both disorders require evaluation of electrolyte panels, renal function, and vitamin D status, with hypomagnesemia often causing functional hypocalcemia due to impaired PTH secretion or action.
Pathophysiological Mechanisms
Hypomagnesemia disrupts parathyroid hormone (PTH) secretion and induces PTH resistance, leading to impaired calcium homeostasis and subsequent hypocalcemia. Magnesium deficiency reduces intracellular magnesium levels, causing altered cellular ion channel activity and impaired release of PTH, which is essential for calcium mobilization from bone and kidney reabsorption. In contrast, hypocalcemia primarily results from inadequate calcium intake, vitamin D deficiency, or parathyroid gland dysfunction, directly affecting serum calcium concentration without initial magnesium involvement.
Treatment and Management Strategies
Treatment of hypomagnesemia primarily involves magnesium supplementation through oral or intravenous routes depending on severity, addressing underlying causes such as alcoholism or gastrointestinal losses. Hypocalcemia management focuses on calcium replacement, either orally for mild cases or intravenously for severe symptoms, along with vitamin D analogs to enhance calcium absorption. Both conditions require monitoring of electrolyte levels and correction of associated factors like hypoparathyroidism or renal impairment to prevent recurrence.
Complications and Prognosis
Hypomagnesemia can lead to severe neuromuscular symptoms such as tetany, seizures, and cardiac arrhythmias, posing a significant risk for sudden cardiac death if untreated. Hypocalcemia primarily results in neuromuscular irritability, including muscle cramps, tetany, and, in severe cases, laryngospasm or seizures, potentially causing respiratory failure. Both conditions require prompt diagnosis and management, as persistent electrolyte imbalances can lead to chronic complications and poor prognosis without adequate treatment.
Prevention and Patient Education
Preventing hypomagnesemia and hypocalcemia involves maintaining balanced dietary intake rich in magnesium- and calcium-containing foods such as leafy greens, nuts, dairy products, and fortified cereals. Patient education should emphasize recognizing early symptoms like muscle cramps, fatigue, and numbness, and the importance of adherence to prescribed supplements or medications. Regular monitoring of serum magnesium and calcium levels is crucial for at-risk individuals, including those with gastrointestinal disorders or on diuretics, to avoid complications.
Hypomagnesemia Infographic
 libterm.com
libterm.com