Keratomalacia is a severe eye disorder caused by vitamin A deficiency, leading to the softening and ulceration of the cornea. If left untreated, it can result in permanent blindness and other serious ocular complications. Explore the rest of the article to understand the symptoms, causes, and effective treatments to protect your vision.
Table of Comparison
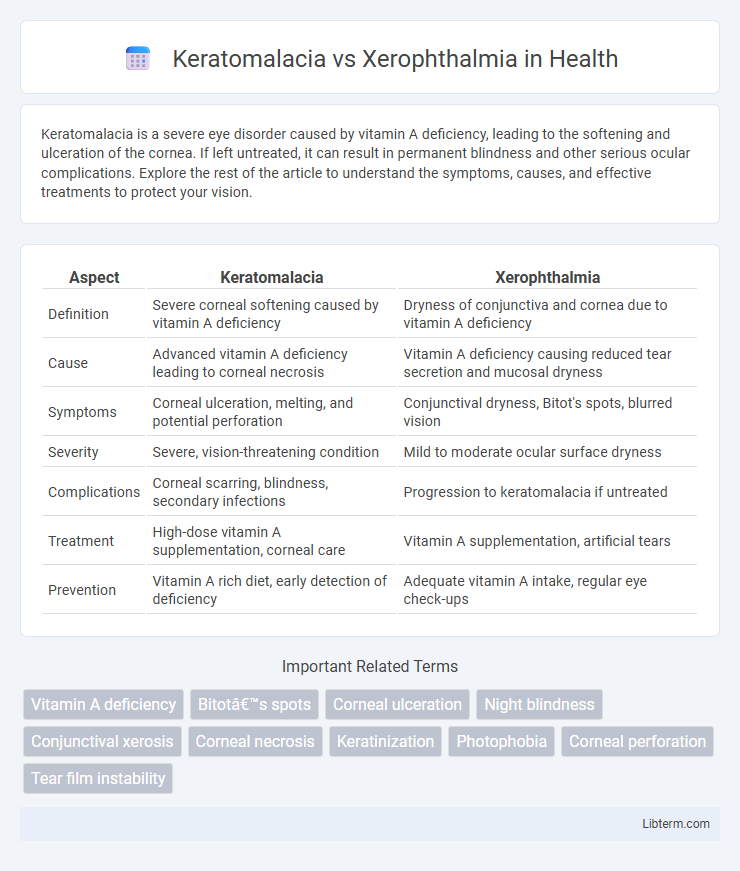
| Aspect | Keratomalacia | Xerophthalmia |
|---|---|---|
| Definition | Severe corneal softening caused by vitamin A deficiency | Dryness of conjunctiva and cornea due to vitamin A deficiency |
| Cause | Advanced vitamin A deficiency leading to corneal necrosis | Vitamin A deficiency causing reduced tear secretion and mucosal dryness |
| Symptoms | Corneal ulceration, melting, and potential perforation | Conjunctival dryness, Bitot's spots, blurred vision |
| Severity | Severe, vision-threatening condition | Mild to moderate ocular surface dryness |
| Complications | Corneal scarring, blindness, secondary infections | Progression to keratomalacia if untreated |
| Treatment | High-dose vitamin A supplementation, corneal care | Vitamin A supplementation, artificial tears |
| Prevention | Vitamin A rich diet, early detection of deficiency | Adequate vitamin A intake, regular eye check-ups |
Introduction to Keratomalacia and Xerophthalmia
Keratomalacia and xerophthalmia are severe ocular conditions caused by vitamin A deficiency, primarily affecting the cornea and conjunctiva. Xerophthalmia represents the early stage characterized by dryness, night blindness, and Bitot's spots, while keratomalacia is the advanced, sight-threatening stage involving corneal softening and ulceration. Both conditions are prevalent in populations with malnutrition and poor vitamin A intake, requiring prompt intervention to prevent irreversible blindness.
Definition and Overview
Keratomalacia is a severe eye disorder characterized by the softening and ulceration of the cornea due to vitamin A deficiency, often leading to blindness if untreated. Xerophthalmia encompasses a spectrum of eye conditions caused by vitamin A deficiency, including dryness of the conjunctiva and cornea, night blindness, and keratomalacia as its most advanced stage. Both conditions primarily affect populations with malnutrition or malabsorption but differ in severity, with xerophthalmia representing early to progressive symptoms and keratomalacia signifying advanced corneal damage.
Etiology and Pathophysiology
Keratomalacia and xerophthalmia are both ocular conditions primarily caused by severe vitamin A deficiency, disrupting normal epithelial cell differentiation in the cornea and conjunctiva. Keratomalacia involves the liquefactive necrosis and softening of the cornea due to advanced vitamin A deficiency, leading to corneal ulceration and potential blindness. Xerophthalmia refers to a spectrum of eye diseases characterized by conjunctival and corneal dryness, with impaired mucous secretion and epithelial keratinization resulting from vitamin A deficiency, often progressing to keratomalacia if untreated.
Vitamin A Deficiency: Core Link
Keratomalacia and xerophthalmia are severe ocular conditions stemming from vitamin A deficiency, with keratomalacia characterized by corneal softening and necrosis, while xerophthalmia primarily involves dryness and thickening of the conjunctiva and cornea. Vitamin A deficiency impairs the production of rhodopsin and disrupts mucin secretion from conjunctival goblet cells, leading to compromised epithelial integrity and increased risk of corneal damage. Early detection and supplementation of vitamin A are critical to prevent progression from xerophthalmia to keratomalacia and subsequent irreversible vision loss.
Clinical Presentation and Symptoms
Keratomalacia presents with severe corneal softening and necrosis, often leading to rapid vision loss and potential corneal perforation. Xerophthalmia primarily manifests as dryness of the conjunctiva and cornea, night blindness, and Bitot's spots, indicating vitamin A deficiency. Both conditions exhibit ocular surface damage, but keratomalacia represents a more advanced, destructive stage of xerophthalmia.
Diagnostic Differences
Keratomalacia is characterized by the liquefactive necrosis of the cornea due to severe vitamin A deficiency, diagnosed primarily through clinical signs such as corneal melting and ulceration, often confirmed by low serum retinol levels. Xerophthalmia, encompassing a spectrum from conjunctival xerosis to Bitot's spots, is identified by ocular surface dryness and keratinization visible during slit-lamp examination combined with evidence of vitamin A deficiency. Diagnostic differentiation hinges on the severity of corneal involvement, with keratomalacia presenting as an advanced, vision-threatening stage, whereas xerophthalmia includes earlier, less destructive manifestations.
Risk Factors and Vulnerable Populations
Keratomalacia and xerophthalmia are severe ocular conditions primarily caused by vitamin A deficiency, with risk factors including malnutrition, poor dietary intake, and chronic infections that impair vitamin A absorption. Vulnerable populations consist mainly of young children in developing countries where vitamin A deficiency is endemic, as well as pregnant and lactating women with insufficient vitamin A intake. Immunocompromised individuals and those with gastrointestinal disorders affecting nutrient absorption are also at heightened risk for these conditions.
Prevention Strategies
Preventing keratomalacia and xerophthalmia primarily involves ensuring adequate vitamin A intake through a diet rich in liver, dairy products, and yellow or green leafy vegetables. Supplementation programs targeting at-risk populations, especially children in developing countries, play a critical role in reducing incidence. Public health initiatives promoting breastfeeding and fortifying staple foods with vitamin A are effective strategies to combat these vitamin A deficiency-related ocular conditions.
Treatment and Management Options
Treatment of keratomalacia involves urgent high-dose vitamin A supplementation to prevent corneal melting and blindness, along with antibiotics to treat secondary infections and lubricants to protect the ocular surface. Xerophthalmia management includes regular vitamin A supplementation, maintenance of eyelid hygiene, use of artificial tears to alleviate dryness, and addressing any underlying nutritional deficiencies to prevent progression to more severe corneal damage. Both conditions require nutritional rehabilitation and monitoring to ensure recovery and avoid irreversible vision loss.
Prognosis and Long-Term Complications
Keratomalacia, a severe form of Vitamin A deficiency, leads to corneal necrosis and rapid vision loss, with a poor prognosis if untreated, often resulting in permanent blindness or corneal perforation. Xerophthalmia encompasses a spectrum of ocular manifestations from Vitamin A deficiency, including night blindness and conjunctival xerosis, with variable prognosis depending on severity and timely intervention. Long-term complications of keratomalacia include corneal scarring and blindness, while xerophthalmia may progress to keratomalacia if untreated, increasing risk of irreversible ocular damage.
Keratomalacia Infographic
 libterm.com
libterm.com