Myocardial infarction occurs when blood flow to a part of the heart is blocked, leading to heart muscle damage. Early recognition of symptoms and prompt treatment are crucial to minimize heart damage and improve outcomes. Explore the rest of this article to understand the causes, symptoms, and effective management of myocardial infarction.
Table of Comparison
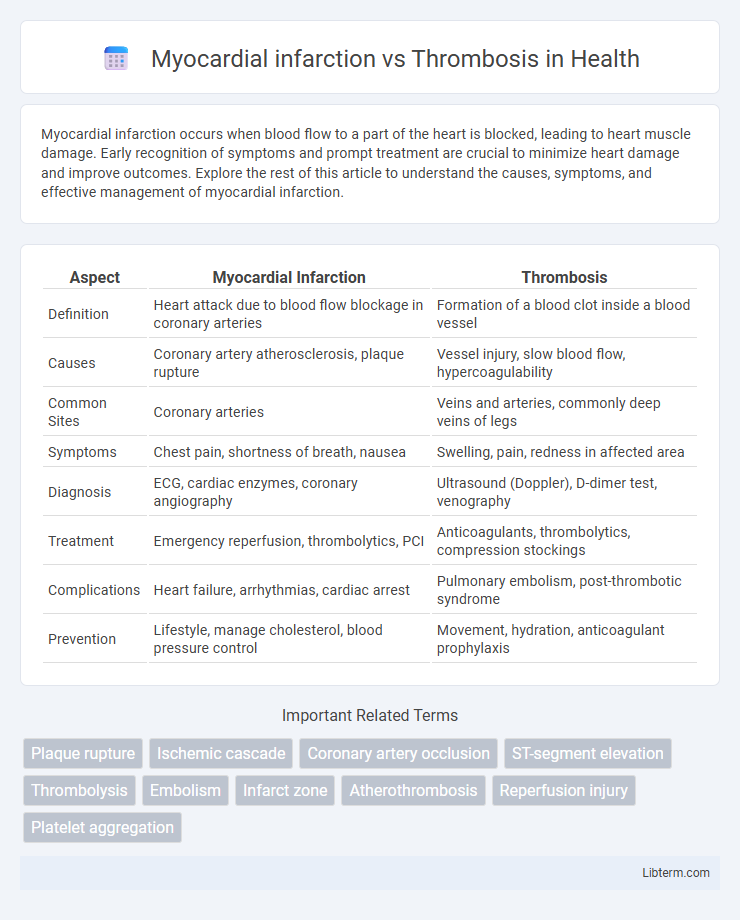
| Aspect | Myocardial Infarction | Thrombosis |
|---|---|---|
| Definition | Heart attack due to blood flow blockage in coronary arteries | Formation of a blood clot inside a blood vessel |
| Causes | Coronary artery atherosclerosis, plaque rupture | Vessel injury, slow blood flow, hypercoagulability |
| Common Sites | Coronary arteries | Veins and arteries, commonly deep veins of legs |
| Symptoms | Chest pain, shortness of breath, nausea | Swelling, pain, redness in affected area |
| Diagnosis | ECG, cardiac enzymes, coronary angiography | Ultrasound (Doppler), D-dimer test, venography |
| Treatment | Emergency reperfusion, thrombolytics, PCI | Anticoagulants, thrombolytics, compression stockings |
| Complications | Heart failure, arrhythmias, cardiac arrest | Pulmonary embolism, post-thrombotic syndrome |
| Prevention | Lifestyle, manage cholesterol, blood pressure control | Movement, hydration, anticoagulant prophylaxis |
Introduction to Myocardial Infarction and Thrombosis
Myocardial infarction (MI) occurs when blood flow to the heart muscle is abruptly blocked, often due to a coronary artery thrombosis, resulting in tissue damage. Thrombosis involves the formation of a blood clot within a blood vessel, which can obstruct blood flow and precipitate cardiovascular events like MI or stroke. Understanding the pathophysiology of thrombosis is critical for diagnosing and managing myocardial infarction effectively.
Definition and Key Differences
Myocardial infarction, commonly known as a heart attack, occurs when blood flow to a part of the heart muscle is blocked, causing tissue damage or necrosis due to oxygen deprivation. Thrombosis refers to the formation of a blood clot within a blood vessel, which can impede blood flow and potentially lead to myocardial infarction if the clot obstructs coronary arteries. The key difference lies in myocardial infarction being an outcome caused by restricted blood supply, while thrombosis is the pathological process that can trigger such an event.
Causes and Risk Factors
Myocardial infarction primarily results from the sudden blockage of coronary arteries due to atherosclerotic plaque rupture and subsequent thrombus formation, leading to impaired blood flow to the heart muscle. Thrombosis is caused by factors outlined in Virchow's triad: endothelial injury, hypercoagulability, and stasis of blood flow, which collectively increase the risk of clot formation in arteries or veins. Key risk factors for myocardial infarction include hypertension, hyperlipidemia, smoking, diabetes, and family history, while thrombosis risk factors encompass prolonged immobility, anticoagulant deficiencies, malignancy, and certain genetic mutations like Factor V Leiden.
Pathophysiology Comparison
Myocardial infarction primarily results from the sudden occlusion of a coronary artery due to the rupture of an atherosclerotic plaque followed by thrombosis formation, leading to ischemia and necrosis of myocardial tissue. Thrombosis involves the formation of a blood clot within the vascular system, often caused by endothelial injury, stasis of blood flow, or hypercoagulability, which can precipitate ischemic events like myocardial infarction if occurring in coronary arteries. The key pathophysiological difference lies in myocardial infarction being an end-organ consequence of coronary thrombosis, whereas thrombosis itself is the acute intravascular clot formation process.
Clinical Presentation and Symptoms
Myocardial infarction typically presents with intense chest pain radiating to the left arm, jaw, or back, accompanied by shortness of breath, diaphoresis, and nausea. In contrast, thrombosis symptoms depend on the affected vessel; arterial thrombosis may cause sudden pain and ischemia, whereas venous thrombosis often presents with swelling, redness, and tenderness in the affected limb. Prompt recognition of these distinct clinical features is critical for accurate diagnosis and timely intervention.
Diagnostic Approaches
Myocardial infarction diagnosis relies on electrocardiograms (ECG), cardiac biomarkers such as troponin levels, and imaging techniques like coronary angiography to identify ischemic damage. Thrombosis diagnosis involves Doppler ultrasound for detecting vessel occlusions, D-dimer blood tests to assess clot presence, and sometimes venography or magnetic resonance imaging (MRI) to locate thrombi. Distinguishing between the two conditions requires integrating clinical evaluation with targeted diagnostic tools to determine the underlying cause of vascular obstruction.
Treatment and Management Strategies
Treatment of myocardial infarction focuses on rapid reperfusion using thrombolytic therapy or percutaneous coronary intervention to restore blood flow and minimize heart muscle damage. Thrombosis management prioritizes anticoagulant medications such as heparin or direct oral anticoagulants to prevent clot expansion and reduce the risk of embolism. Both conditions require long-term strategies including antiplatelet therapy, lifestyle modification, and monitoring to prevent recurrence and improve cardiovascular outcomes.
Prognosis and Complications
Myocardial infarction prognosis depends on the extent of heart muscle damage and timely intervention, with complications including heart failure, arrhythmias, and cardiogenic shock. Thrombosis prognosis varies based on the location and size of the clot, with potential complications such as embolism, tissue ischemia, and organ damage. Both conditions require prompt diagnosis and management to reduce morbidity and mortality risks.
Prevention and Lifestyle Modifications
Preventing myocardial infarction and thrombosis involves managing key risk factors such as hypertension, hyperlipidemia, diabetes, and smoking through lifestyle modifications like a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins. Regular physical activity, maintaining a healthy weight, stress reduction, and avoiding tobacco use significantly reduce the incidence of arterial clot formation and coronary artery blockages. Medications such as antiplatelets or anticoagulants may be prescribed alongside lifestyle changes to further lower the risk of thrombosis and subsequent myocardial infarction.
Summary and Key Takeaways
Myocardial infarction occurs due to the obstruction of coronary arteries, commonly caused by thrombosis, which is the formation of a blood clot within a vessel. Thrombosis, while a broader term, can lead to myocardial infarction when it disrupts blood flow to the heart muscle, resulting in tissue damage or necrosis. Key takeaways include understanding that thrombosis is a primary cause of myocardial infarction and early detection and treatment of thrombotic events are critical to preventing heart damage.
Myocardial infarction Infographic
 libterm.com
libterm.com