Sarcopenia and osteoporosis are interrelated conditions characterized by the loss of muscle mass and bone density, respectively, significantly increasing the risk of fractures and mobility issues. Understanding the underlying causes, symptoms, and prevention strategies is crucial for maintaining your overall musculoskeletal health as you age. Explore the rest of the article to learn effective ways to combat these conditions and improve your quality of life.
Table of Comparison
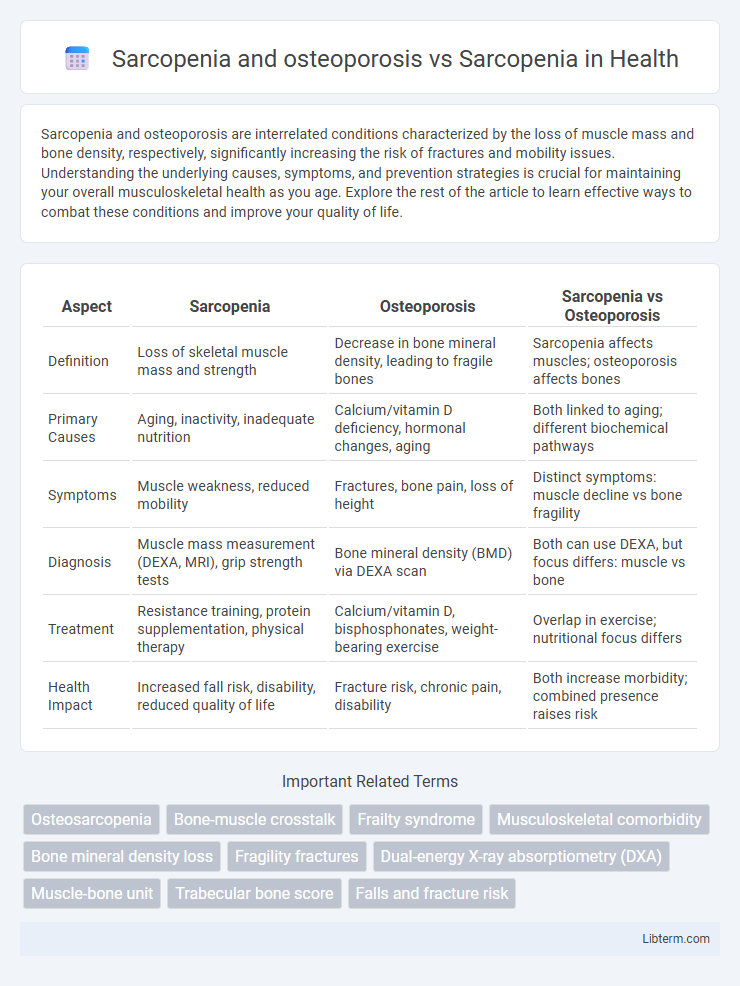
| Aspect | Sarcopenia | Osteoporosis | Sarcopenia vs Osteoporosis |
|---|---|---|---|
| Definition | Loss of skeletal muscle mass and strength | Decrease in bone mineral density, leading to fragile bones | Sarcopenia affects muscles; osteoporosis affects bones |
| Primary Causes | Aging, inactivity, inadequate nutrition | Calcium/vitamin D deficiency, hormonal changes, aging | Both linked to aging; different biochemical pathways |
| Symptoms | Muscle weakness, reduced mobility | Fractures, bone pain, loss of height | Distinct symptoms: muscle decline vs bone fragility |
| Diagnosis | Muscle mass measurement (DEXA, MRI), grip strength tests | Bone mineral density (BMD) via DEXA scan | Both can use DEXA, but focus differs: muscle vs bone |
| Treatment | Resistance training, protein supplementation, physical therapy | Calcium/vitamin D, bisphosphonates, weight-bearing exercise | Overlap in exercise; nutritional focus differs |
| Health Impact | Increased fall risk, disability, reduced quality of life | Fracture risk, chronic pain, disability | Both increase morbidity; combined presence raises risk |
Understanding Sarcopenia: Definition and Key Features
Sarcopenia is a progressive loss of skeletal muscle mass and strength, significantly impacting physical function and increasing the risk of falls and fractures. Osteoporosis, characterized by reduced bone mineral density and bone quality, often coexists with sarcopenia, intensifying musculoskeletal decline. Understanding sarcopenia involves recognizing key features such as muscle atrophy, decreased muscle performance, and impaired mobility essential for targeted interventions and improved patient outcomes.
What is Osteoporosis? Core Concepts and Mechanisms
Osteoporosis is a progressive bone disease characterized by decreased bone mass and microarchitectural deterioration, leading to increased fracture risk. The core mechanisms involve an imbalance between bone resorption by osteoclasts and bone formation by osteoblasts, often exacerbated by hormonal changes, nutrient deficiencies, and aging. Unlike sarcopenia, which primarily affects muscle mass and function, osteoporosis specifically targets bone density and structural integrity, though both conditions frequently coexist in the elderly, contributing to frailty.
Sarcopenia vs Osteoporosis: Distinct Conditions Explained
Sarcopenia and osteoporosis are distinct conditions affecting older adults, with sarcopenia characterized by the progressive loss of muscle mass and function, while osteoporosis involves decreased bone density and increased fracture risk. Sarcopenia primarily impairs mobility and strength, whereas osteoporosis increases vulnerability to bone fractures, particularly in the hip, spine, and wrist. Understanding these differences is critical for targeted prevention, diagnosis, and treatment strategies in aging populations.
The Link Between Sarcopenia and Osteoporosis: Pathophysiology
Sarcopenia and osteoporosis share a common pathophysiological link through the disruption of muscle-bone crosstalk, involving decreased production of myokines and osteokines that regulate musculoskeletal homeostasis. Both conditions are influenced by aging-related hormonal changes, chronic inflammation, and inadequate nutrient intake, leading to impaired muscle protein synthesis and bone remodeling. Understanding this interplay highlights the importance of targeting molecular pathways like the Wnt/b-catenin signaling and oxidative stress to simultaneously manage sarcopenia and osteoporosis effectively.
Prevalence and Risk Factors: Comparing Sarcopenia and Osteoporosis
Sarcopenia affects approximately 10% of adults over 60, while osteoporosis impacts nearly 20% of individuals in the same age group, highlighting higher prevalence in bone density loss. Risk factors for sarcopenia include physical inactivity, chronic inflammation, and inadequate protein intake, whereas osteoporosis risk factors emphasize calcium/vitamin D deficiency, hormonal changes, and advanced age. Both conditions share common contributors such as aging and sedentary lifestyle but differ in metabolic pathways influencing muscle mass versus bone mineral density.
Shared Consequences: Frailty, Falls, and Disability
Sarcopenia and osteoporosis both contribute significantly to frailty, increasing vulnerability to falls and subsequent disabilities in older adults. Sarcopenia leads to muscle weakness and reduced physical function, while osteoporosis compromises bone strength, collectively heightening fracture risk. Addressing these conditions together is essential to prevent mobility decline and improve quality of life in aging populations.
Diagnostic Criteria: Assessing Muscle and Bone Health
Diagnostic criteria for sarcopenia focus on measuring muscle mass, strength, and physical performance using tools such as DXA scans, grip strength tests, and gait speed assessments. Osteoporosis diagnosis relies primarily on bone mineral density (BMD) evaluation through DXA scans, with T-scores indicating bone fragility. Assessing both muscle and bone health together provides a comprehensive understanding of musculoskeletal deterioration and guides targeted interventions.
Treatment Strategies: Sarcopenia Alone vs Combined Conditions
Treatment strategies for sarcopenia alone primarily involve resistance training, protein supplementation, and vitamin D to enhance muscle strength and mass. In cases of combined sarcopenia and osteoporosis, interventions include these approaches along with anti-osteoporotic medications such as bisphosphonates or denosumab to improve bone density and reduce fracture risk. Tailored rehabilitation programs and nutritional optimization are critical in managing both conditions effectively to improve overall musculoskeletal health.
Preventive Measures: Nutrition, Exercise, and Lifestyle
Preventive measures for sarcopenia and osteoporosis emphasize adequate nutrition rich in protein, calcium, and vitamin D to support muscle mass and bone density. Regular weight-bearing and resistance exercises enhance muscle strength and stimulate bone remodeling, reducing the risk of fractures and functional decline. Lifestyle factors such as avoiding smoking, limiting alcohol intake, and maintaining a healthy body weight play a crucial role in preventing both conditions.
Future Directions: Integrated Management and Research in Musculoskeletal Aging
Future directions in musculoskeletal aging emphasize integrated management strategies combining sarcopenia and osteoporosis treatments to improve patient outcomes. Research focuses on understanding shared molecular pathways such as inflammation and hormonal changes to develop dual-action therapies. Advances in personalized medicine and biomarker discovery aim to optimize prevention, diagnosis, and intervention for individuals with concurrent muscle and bone degeneration.
Sarcopenia and osteoporosis Infographic
 libterm.com
libterm.com