A brain abscess is a serious medical condition where pus collects in the brain tissue due to infection, often caused by bacteria or fungi. Symptoms typically include headache, fever, neurological deficits, and altered mental status, requiring prompt diagnosis with imaging such as MRI or CT scan. Explore the rest of the article to understand the causes, treatment options, and how timely intervention can protect your health.
Table of Comparison
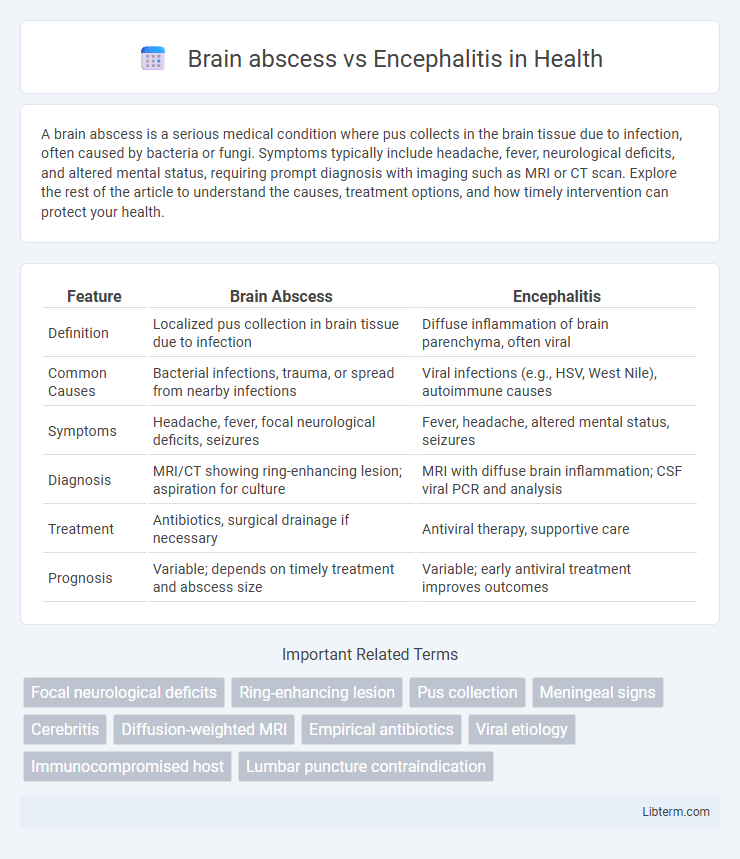
| Feature | Brain Abscess | Encephalitis |
|---|---|---|
| Definition | Localized pus collection in brain tissue due to infection | Diffuse inflammation of brain parenchyma, often viral |
| Common Causes | Bacterial infections, trauma, or spread from nearby infections | Viral infections (e.g., HSV, West Nile), autoimmune causes |
| Symptoms | Headache, fever, focal neurological deficits, seizures | Fever, headache, altered mental status, seizures |
| Diagnosis | MRI/CT showing ring-enhancing lesion; aspiration for culture | MRI with diffuse brain inflammation; CSF viral PCR and analysis |
| Treatment | Antibiotics, surgical drainage if necessary | Antiviral therapy, supportive care |
| Prognosis | Variable; depends on timely treatment and abscess size | Variable; early antiviral treatment improves outcomes |
Introduction to Brain Abscess and Encephalitis
Brain abscess is a localized collection of pus within the brain parenchyma caused by bacterial or fungal infection, leading to focal neurological symptoms and increased intracranial pressure. Encephalitis, on the other hand, is a diffuse inflammation of the brain tissue typically resulting from viral infections, manifesting with altered mental status, seizures, and systemic symptoms like fever. Distinguishing between these two conditions requires neuroimaging and cerebrospinal fluid analysis to guide appropriate antimicrobial or antiviral therapy.
Definition and Overview
A brain abscess is a localized collection of pus within the brain tissue caused by bacterial or fungal infection, leading to a focal, encapsulated inflammatory lesion. Encephalitis refers to diffuse inflammation of the brain parenchyma, usually due to viral infections such as herpes simplex virus, resulting in widespread neuronal damage and dysfunction. Both conditions require prompt diagnosis and treatment but differ significantly in pathophysiology, clinical presentation, and imaging characteristics.
Etiology and Causes
Brain abscess is primarily caused by bacterial or fungal infections that result in a localized collection of pus within the brain parenchyma, often stemming from contiguous infections such as otitis media, sinusitis, or hematogenous spread from distant sites like endocarditis. Encephalitis, in contrast, is mainly triggered by viral infections including herpes simplex virus, arboviruses, and enteroviruses, leading to diffuse inflammation of the brain tissue. Both conditions reflect distinct pathophysiological mechanisms where brain abscesses involve focal suppurative processes, whereas encephalitis involves widespread inflammatory damage primarily due to infectious agents.
Pathophysiology: How Each Condition Develops
Brain abscess develops through localized infection and inflammation resulting from bacterial or fungal invasion, leading to a pus-filled cavity within the brain parenchyma. In contrast, encephalitis arises from direct viral infection or autoimmune response causing widespread inflammation of the brain tissue. The distinct pathophysiological processes involve abscess formation encapsulated by a collagenous capsule in brain abscess, whereas encephalitis features diffuse neuronal damage and edema.
Key Differences in Symptoms
Brain abscess typically presents with localized neurological deficits, severe headache, fever, and signs of increased intracranial pressure such as vomiting and altered consciousness. Encephalitis commonly manifests with diffuse brain inflammation symptoms including fever, headache, altered mental status, seizures, and behavioral changes. While brain abscess symptoms are more focal and progressive due to localized infection, encephalitis usually causes widespread cerebral dysfunction with rapid onset of neuropsychiatric symptoms.
Diagnostic Approaches and Imaging
Brain abscess diagnosis relies heavily on contrast-enhanced MRI and CT scans, revealing ring-enhancing lesions with central necrosis, while diffusion-weighted imaging (DWI) helps differentiate abscess from cystic tumors. Encephalitis diagnosis incorporates MRI showing diffuse or focal hyperintensities, especially in the temporal lobes in HSV encephalitis, alongside cerebrospinal fluid analysis identifying viral antibodies or PCR confirmation. Both conditions often require EEG for seizure activity assessment and lumbar puncture for CSF examination to distinguish infectious etiologies.
Treatment Strategies and Management
Treatment strategies for brain abscess primarily involve surgical intervention such as aspiration or excision combined with prolonged intravenous antibiotic therapy targeting common pathogens like Streptococcus and anaerobes. Encephalitis management focuses on antiviral medications, especially acyclovir for herpes simplex virus, alongside supportive care including corticosteroids to reduce cerebral edema and control seizures. Early diagnosis and tailored treatment based on etiology and imaging findings are critical to improving outcomes in both conditions.
Complications and Prognosis
Brain abscess complications often include increased intracranial pressure, seizures, and potential rupture causing ventriculitis or meningitis, with prognosis heavily dependent on timely surgical drainage and antimicrobial therapy. Encephalitis can lead to neurological deficits, cognitive impairments, or persistent seizures, and its prognosis varies widely based on the causative agent, patient age, and immune status. Both conditions require early diagnosis and targeted treatment to minimize mortality and long-term neurological sequelae.
Prevention and Risk Factors
Brain abscess risk factors include immunosuppression, head trauma, and chronic ear or sinus infections, while encephalitis often stems from viral infections such as herpes simplex virus or mosquito-borne viruses. Prevention strategies for brain abscess focus on prompt treatment of infections and maintaining strong immune health, whereas encephalitis prevention involves vaccination, mosquito control, and avoiding exposure to infectious agents. Both conditions require minimizing exposure to their respective infectious sources and managing underlying health issues to reduce risk.
Summary: Differentiating Brain Abscess vs Encephalitis
Brain abscess presents as a focal intracerebral infection typically characterized by a localized pus collection, commonly identified via contrast-enhanced MRI showing ring-enhancing lesions. Encephalitis involves diffuse inflammation of the brain parenchyma, often viral in origin, with clinical features such as altered mental status, seizures, and diffuse brain swelling visible on imaging. Differentiation hinges on imaging patterns, clinical presentation, cerebrospinal fluid analysis, and etiology, with brain abscess requiring surgical drainage and antibiotics, whereas encephalitis primarily necessitates antiviral therapy and supportive care.
Brain abscess Infographic
 libterm.com
libterm.com