Osteomalacia is a bone disorder characterized by the softening of bones due to defective bone mineralization, often caused by vitamin D deficiency. This condition leads to bone pain, muscle weakness, and an increased risk of fractures, significantly affecting your mobility and quality of life. Explore the rest of this article to understand the causes, symptoms, and effective treatments for osteomalacia.
Table of Comparison
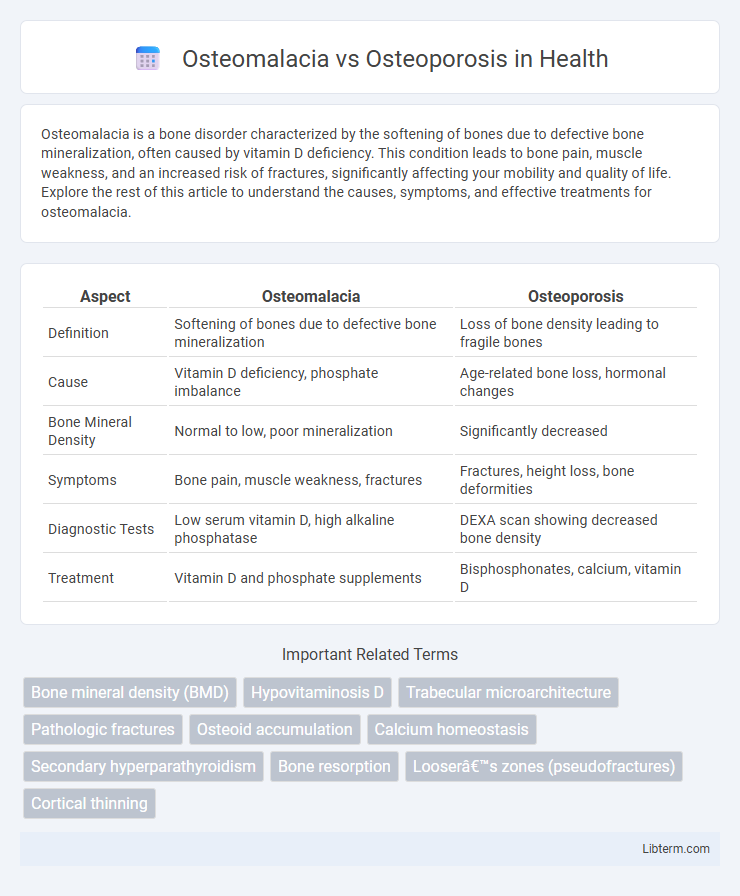
| Aspect | Osteomalacia | Osteoporosis |
|---|---|---|
| Definition | Softening of bones due to defective bone mineralization | Loss of bone density leading to fragile bones |
| Cause | Vitamin D deficiency, phosphate imbalance | Age-related bone loss, hormonal changes |
| Bone Mineral Density | Normal to low, poor mineralization | Significantly decreased |
| Symptoms | Bone pain, muscle weakness, fractures | Fractures, height loss, bone deformities |
| Diagnostic Tests | Low serum vitamin D, high alkaline phosphatase | DEXA scan showing decreased bone density |
| Treatment | Vitamin D and phosphate supplements | Bisphosphonates, calcium, vitamin D |
Understanding Osteomalacia and Osteoporosis
Osteomalacia is characterized by the softening of bones due to defective bone mineralization, primarily caused by vitamin D deficiency or phosphate imbalance, leading to bone pain and muscle weakness. Osteoporosis involves decreased bone density and structural deterioration, increasing fracture risk, often linked to hormonal changes such as reduced estrogen levels in postmenopausal women. Understanding the distinct pathophysiology of osteomalacia and osteoporosis aids in accurate diagnosis and targeted treatment strategies for bone health management.
Key Differences in Pathophysiology
Osteomalacia is characterized by defective bone mineralization due to vitamin D deficiency, leading to soft and weak bones, whereas osteoporosis involves reduced bone mass and microarchitectural deterioration, resulting in fragile and porous bones. The primary pathophysiological cause of osteomalacia is impaired calcium and phosphate deposition in the bone matrix, while osteoporosis stems from an imbalance between bone resorption and bone formation, favoring resorption. Unlike osteomalacia, which presents with bone pain and muscle weakness, osteoporosis is typically asymptomatic until fractures occur.
Causes and Risk Factors
Osteomalacia primarily results from vitamin D deficiency, leading to impaired bone mineralization, while osteoporosis is caused by an imbalance between bone resorption and formation, often due to aging, hormonal changes, or calcium deficiency. Risk factors for osteomalacia include inadequate sunlight exposure, malabsorption disorders, and certain medications affecting vitamin D metabolism. Osteoporosis risk factors encompass postmenopausal status, advanced age, family history, low body weight, smoking, and prolonged corticosteroid use.
Symptoms and Clinical Presentation
Osteomalacia primarily presents with diffuse bone pain, muscle weakness, and difficulty walking due to defective bone mineralization caused by vitamin D deficiency. Osteoporosis is often asymptomatic until a fracture occurs, typically resulting in sudden bone pain, height loss, and spinal deformities such as kyphosis. Both conditions increase fracture risk, but osteomalacia's symptoms are more related to bone softening, while osteoporosis is characterized by decreased bone density and fragility.
Diagnostic Methods and Criteria
Osteomalacia diagnosis involves measuring serum levels of vitamin D, calcium, and phosphorus, along with elevated alkaline phosphatase and bone biopsies revealing defective mineralization. Osteoporosis is primarily diagnosed using dual-energy X-ray absorptiometry (DEXA) scans showing a T-score <= -2.5 at the lumbar spine or hip, indicating decreased bone mineral density. While both conditions affect bone strength, osteomalacia results from impaired bone mineralization, and osteoporosis stems from reduced bone mass and microarchitectural deterioration.
Bone Density and Structural Changes
Osteomalacia presents with softened bones due to defective bone mineralization, leading to decreased bone density but primarily affects bone quality by causing inadequate calcium and phosphate deposition. Osteoporosis is characterized by reduced bone mass and microarchitectural deterioration, resulting in porous, fragile bones with significantly diminished bone density and increased fracture risk. Structural changes in osteomalacia involve softened, pliable bones prone to deformities, whereas osteoporosis leads to thinning of trabeculae and cortical bone, compromising bone strength without affecting the mineralization process.
Treatment Approaches and Management
Osteomalacia treatment primarily involves vitamin D and calcium supplementation to correct mineral deficiencies and enhance bone mineralization, while addressing underlying causes such as malabsorption or inadequate sun exposure. Osteoporosis management emphasizes bisphosphonates, selective estrogen receptor modulators (SERMs), and lifestyle modifications including weight-bearing exercise and fall prevention to reduce fracture risk. Both conditions require ongoing monitoring of bone density and metabolic parameters to optimize therapeutic outcomes and prevent complications.
Nutritional and Lifestyle Interventions
Osteomalacia requires increased vitamin D, calcium, and phosphate intake to enhance bone mineralization, with sunlight exposure playing a crucial role in vitamin D synthesis. Osteoporosis management emphasizes calcium and vitamin D supplementation combined with weight-bearing exercises to improve bone density and reduce fracture risk. Both conditions benefit from a balanced diet rich in essential nutrients and lifestyle modifications that promote bone health and prevent further deterioration.
Complications and Long-term Outlook
Osteomalacia leads to bone softening due to defective mineralization, increasing the risk of fractures and muscular weakness, which can cause persistent pain and limited mobility. Osteoporosis causes reduced bone density and structural deterioration, significantly raising the likelihood of fractures, particularly in the hip, spine, and wrist, often resulting in chronic pain and disability. Long-term outcomes of osteomalacia improve with vitamin D and calcium supplementation, while osteoporosis often requires ongoing treatment to slow bone loss and prevent fractures, with complications potentially leading to decreased quality of life and increased morbidity.
Prevention Strategies for Bone Health
Osteomalacia prevention centers on ensuring adequate vitamin D intake through sunlight exposure, diet rich in fatty fish, fortified foods, and supplements to promote proper bone mineralization. Osteoporosis prevention emphasizes maintaining sufficient calcium levels, engaging in weight-bearing exercises, and avoiding smoking and excessive alcohol consumption to preserve bone density. Both conditions benefit from regular bone density screenings and lifestyle modifications to enhance skeletal strength and reduce fracture risk.
Osteomalacia Infographic
 libterm.com
libterm.com