Neutropenia and agranulocytosis are serious blood disorders characterized by abnormally low levels of neutrophils, leading to increased vulnerability to infections. Effective diagnosis and management are crucial to prevent life-threatening complications and support your immune system's ability to fight off pathogens. Dive into the rest of this article to understand the causes, symptoms, and treatments that can help safeguard your health.
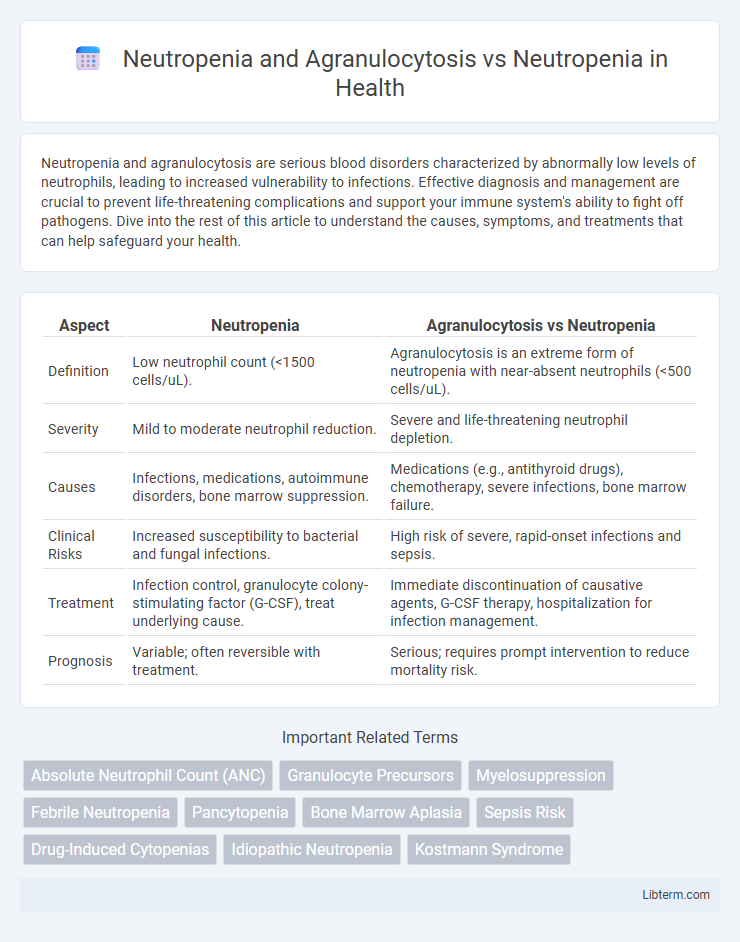
Table of Comparison
| Aspect | Neutropenia | Agranulocytosis vs Neutropenia |
|---|---|---|
| Definition | Low neutrophil count (<1500 cells/uL). | Agranulocytosis is an extreme form of neutropenia with near-absent neutrophils (<500 cells/uL). |
| Severity | Mild to moderate neutrophil reduction. | Severe and life-threatening neutrophil depletion. |
| Causes | Infections, medications, autoimmune disorders, bone marrow suppression. | Medications (e.g., antithyroid drugs), chemotherapy, severe infections, bone marrow failure. |
| Clinical Risks | Increased susceptibility to bacterial and fungal infections. | High risk of severe, rapid-onset infections and sepsis. |
| Treatment | Infection control, granulocyte colony-stimulating factor (G-CSF), treat underlying cause. | Immediate discontinuation of causative agents, G-CSF therapy, hospitalization for infection management. |
| Prognosis | Variable; often reversible with treatment. | Serious; requires prompt intervention to reduce mortality risk. |
Overview of Neutropenia
Neutropenia is a hematological condition characterized by an abnormally low concentration of neutrophils, typically defined as fewer than 1,500 neutrophils per microliter of blood, increasing susceptibility to infections. Agranulocytosis represents a severe form of neutropenia marked by an almost complete absence of granulocytes, especially neutrophils, often dropping below 500 cells per microliter and posing a critical risk for life-threatening infections. Understanding these distinctions is essential for appropriate diagnosis, clinical management, and therapeutic interventions in patients presenting with compromised immune defenses.
Defining Agranulocytosis
Agranulocytosis is a severe form of neutropenia characterized by an extremely low count of neutrophils, often below 500 cells per microliter, which significantly increases the risk of life-threatening infections. Unlike general neutropenia, agranulocytosis involves a near-complete depletion of granulocytes, particularly neutrophils, impacting the body's primary defense against bacterial and fungal pathogens. Accurate diagnosis requires hematological analysis and is critical for prompt treatment to prevent complications associated with this acute hematologic condition.
Causes of Neutropenia
Neutropenia is primarily caused by factors such as bone marrow suppression due to chemotherapy, autoimmune disorders like lupus, severe infections, and certain medications including antipsychotics and antibiotics. Agranulocytosis, a severe form of neutropenia characterized by an almost complete absence of neutrophils, often results from drug-induced bone marrow toxicity, particularly from antithyroid drugs, sulfonamides, or chemotherapy agents. Genetic disorders, vitamin deficiencies (B12, folate), and viral infections (HIV, hepatitis) also contribute to the development of neutropenia, highlighting the diversity of its etiologies.
Causes of Agranulocytosis
Agranulocytosis is a severe form of neutropenia characterized by an extremely low granulocyte count, primarily neutrophils, which significantly increases infection risk. The causes of agranulocytosis often include adverse drug reactions, such as those induced by antithyroid drugs, antibiotics, and chemotherapy agents, as well as autoimmune disorders and bone marrow failure syndromes. Unlike general neutropenia, agranulocytosis typically results from direct toxic effects on bone marrow progenitor cells or immune-mediated destruction of neutrophils.
Pathophysiological Differences
Neutropenia involves a decreased number of neutrophils, typically due to impaired production or increased destruction, whereas agranulocytosis represents a severe form of neutropenia characterized by near-complete absence of granulocytes, especially neutrophils, leading to high infection risk. The pathophysiology of neutropenia arises from bone marrow suppression, autoimmune destruction, or chemotherapy-induced toxicity, while agranulocytosis often results from drug-induced marrow failure or immune-mediated mechanisms targeting myeloid precursor cells. Understanding these distinct mechanisms is critical for differential diagnosis and targeted treatment strategies in hematological disorders.
Clinical Manifestations
Neutropenia presents with increased susceptibility to bacterial and fungal infections, characterized by fever, chills, and sore throat, reflecting a reduced neutrophil count below 1,500 cells/uL. Agranulocytosis is a severe form of neutropenia with neutrophil levels dropping below 100 cells/uL, causing rapid onset of severe infections, mucosal ulcerations, and sepsis risk. Clinical manifestations in agranulocytosis are more acute and pronounced, often requiring immediate medical intervention due to the critical immune deficiency.
Diagnostic Criteria and Laboratory Evaluation
Neutropenia is diagnosed by an absolute neutrophil count (ANC) below 1,500 cells/uL, whereas agranulocytosis is a severe form of neutropenia with ANC below 500 cells/uL, indicating a critical reduction in neutrophils. Laboratory evaluation includes complete blood count (CBC) with differential to quantify neutrophil levels, bone marrow biopsy for etiology assessment, and screening for infections or drug-induced causes. Monitoring neutrophil recovery and identifying underlying conditions is essential for differentiating mild neutropenia from agranulocytosis and guiding treatment strategies.
Complications and Prognosis
Neutropenia and agranulocytosis both involve reduced neutrophil counts, with agranulocytosis representing a more severe form marked by critically low neutrophils, leading to higher risks of severe infections and sepsis. Complications of neutropenia include frequent bacterial and fungal infections, delayed wound healing, and systemic inflammatory responses, while agranulocytosis significantly increases susceptibility to life-threatening infections due to near-complete neutrophil depletion. Prognosis in neutropenia depends on the underlying cause and severity, with transient forms often resolving without lasting effects, whereas agranulocytosis requires prompt treatment to prevent fatal outcomes, frequently involving bone marrow recovery interventions and infection management.
Treatment Approaches: Neutropenia vs Agranulocytosis
Treatment approaches for neutropenia primarily involve addressing the underlying cause and may include growth factors such as granulocyte colony-stimulating factor (G-CSF) to stimulate neutrophil production. Agranulocytosis, a severe form of neutropenia characterized by an almost complete absence of neutrophils, requires more aggressive management including immediate cessation of the offending drug, broad-spectrum antibiotics to prevent infections, and often hospitalization for close monitoring. Both conditions benefit from supportive care, but agranulocytosis demands rapid intervention due to its heightened risk of life-threatening infections.
Prevention and Patient Management Strategies
Prevention of neutropenia and agranulocytosis centers on regular blood count monitoring, avoiding known drug triggers, and prompt treatment of infections to reduce complications. Patient management involves individualized medication adjustments, use of granulocyte colony-stimulating factor (G-CSF) to stimulate white blood cell production, and strict hygiene practices to minimize infection risk. Early recognition and education on warning signs empower patients to seek timely care, improving outcomes in neutropenic conditions.
Neutropenia and Agranulocytosis Infographic
 libterm.com
libterm.com