Dehydration occurs when your body loses more fluids than it takes in, leading to impaired bodily functions and symptoms such as dizziness, dry mouth, and fatigue. Proper hydration is essential for maintaining energy levels, supporting organ function, and preventing serious complications. Discover effective ways to recognize, prevent, and treat dehydration in the rest of this article.
Table of Comparison
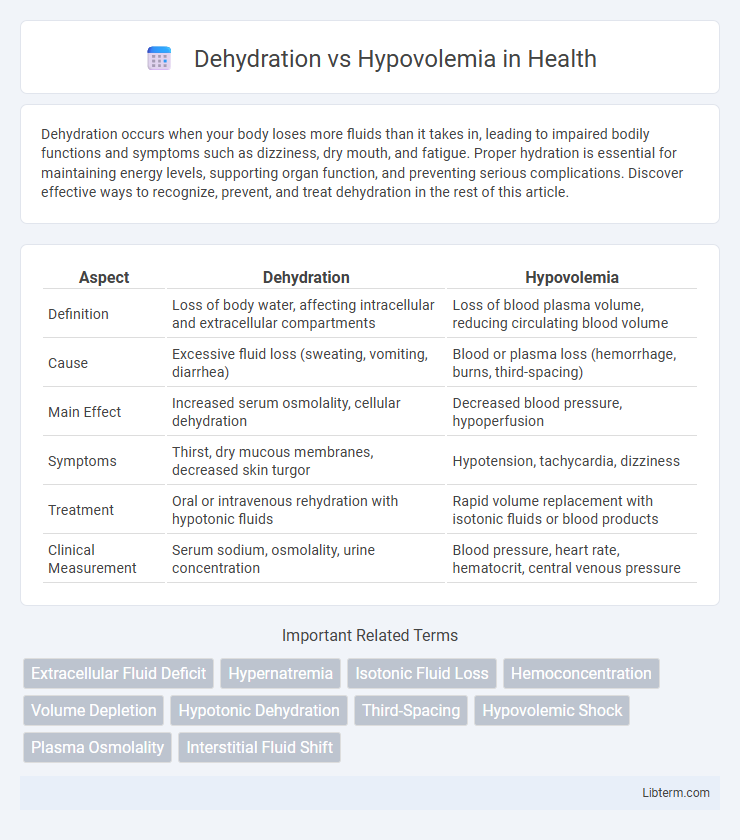
| Aspect | Dehydration | Hypovolemia |
|---|---|---|
| Definition | Loss of body water, affecting intracellular and extracellular compartments | Loss of blood plasma volume, reducing circulating blood volume |
| Cause | Excessive fluid loss (sweating, vomiting, diarrhea) | Blood or plasma loss (hemorrhage, burns, third-spacing) |
| Main Effect | Increased serum osmolality, cellular dehydration | Decreased blood pressure, hypoperfusion |
| Symptoms | Thirst, dry mucous membranes, decreased skin turgor | Hypotension, tachycardia, dizziness |
| Treatment | Oral or intravenous rehydration with hypotonic fluids | Rapid volume replacement with isotonic fluids or blood products |
| Clinical Measurement | Serum sodium, osmolality, urine concentration | Blood pressure, heart rate, hematocrit, central venous pressure |
Introduction to Dehydration and Hypovolemia
Dehydration refers to the excessive loss of body water, leading to an imbalance in fluid and electrolytes, while hypovolemia specifically denotes a decreased volume of circulating blood plasma. Both conditions result in impaired cellular function and can cause symptoms like dizziness, hypotension, and tachycardia, but their underlying mechanisms differ. Recognizing the distinctions between dehydration and hypovolemia is crucial for accurate diagnosis and targeted treatment in clinical practice.
Definitions: Dehydration vs Hypovolemia
Dehydration refers to the excessive loss of body water, leading to an imbalance in fluid levels primarily affecting intracellular compartments. Hypovolemia involves a decreased volume of circulating blood plasma, causing insufficient perfusion and oxygen delivery to tissues. While dehydration centers on water deficit, hypovolemia emphasizes a reduction in overall blood volume, including both water and electrolytes.
Causes and Risk Factors
Dehydration primarily results from excessive fluid loss due to factors such as prolonged sweating, vomiting, diarrhea, and inadequate fluid intake, while hypovolemia is caused by significant blood or fluid volume loss from hemorrhage, burns, or severe dehydration. Risk factors for dehydration include elderly age, chronic illnesses, and high environmental temperatures, whereas hypovolemia risk increases with trauma, major surgery, and conditions causing internal bleeding or plasma loss. Understanding these distinct causes and risk factors is critical for targeted clinical assessment and effective treatment.
Pathophysiology: How Each Condition Develops
Dehydration results from excessive loss of body water, leading to hyperosmolarity and cellular shrinkage as water shifts from intracellular to extracellular compartments. Hypovolemia develops due to significant reduction in intravascular fluid volume caused by factors such as hemorrhage, fluid losses, or inadequate fluid intake, impairing tissue perfusion and oxygen delivery. Both conditions disrupt fluid homeostasis but differ fundamentally in whether total body water or blood volume is primarily affected.
Common Signs and Symptoms
Common signs and symptoms of dehydration include dry mouth, excessive thirst, dark yellow urine, and dizziness. Hypovolemia typically presents with rapid heartbeat, low blood pressure, cold clammy skin, and decreased urine output. Both conditions may cause confusion and weakness, but hypovolemia often leads to more severe circulatory collapse requiring urgent medical intervention.
Diagnostic Criteria and Clinical Assessment
Dehydration primarily involves the loss of total body water leading to hypernatremia, diagnosed through elevated serum sodium levels above 145 mEq/L, increased serum osmolality, and clinical signs such as dry mucous membranes and decreased skin turgor. Hypovolemia reflects a decrease in intravascular volume, often diagnosed by low blood pressure, tachycardia, reduced central venous pressure, and laboratory findings including elevated blood urea nitrogen to creatinine ratio greater than 20:1. Clinical assessment differentiates these conditions by measuring fluid status through vital signs, laboratory tests, and physical examination focusing on volume depletion versus pure water loss.
Key Differences Between Dehydration and Hypovolemia
Dehydration primarily refers to the excessive loss of body water, leading to an increase in serum osmolarity and cellular shrinkage, whereas hypovolemia involves a decrease in circulating blood volume, affecting blood pressure and organ perfusion. Dehydration typically results from inadequate water intake or excessive water loss through sweating or diarrhea, while hypovolemia is often caused by hemorrhage, fluid shifts, or severe dehydration that reduces plasma volume. Clinically, dehydration presents with thirst, dry mucous membranes, and elevated serum sodium, whereas hypovolemia manifests with hypotension, tachycardia, and signs of poor peripheral perfusion.
Treatment Approaches and Management Strategies
Treatment of dehydration centers on oral rehydration solutions or intravenous fluids to restore intracellular fluid balance, with mild cases managed by increasing oral intake of water and electrolytes. Hypovolemia requires rapid intravenous administration of isotonic crystalloids like normal saline or lactated Ringer's solution to restore circulating blood volume and prevent shock. Continuous monitoring of vital signs, urine output, and electrolyte levels guides fluid replacement therapy and addresses underlying causes for effective management of both conditions.
Prevention Tips and Best Practices
Effective prevention of dehydration involves regular intake of fluids, especially water, balanced with electrolyte-rich drinks to maintain hydration and electrolyte levels. For hypovolemia, avoiding excessive blood loss and managing underlying conditions such as bleeding disorders or severe dehydration is crucial to preserve blood volume. Monitoring vital signs and promptly treating symptoms like dizziness or rapid heartbeat help in early detection and prevention of complications associated with both dehydration and hypovolemia.
When to Seek Medical Attention
Seek medical attention urgently for dehydration if symptoms include persistent dizziness, confusion, rapid heartbeat, or inability to keep fluids down, as these indicate severe fluid loss affecting vital functions. Hypovolemia requires immediate emergency care when signs such as low blood pressure, cold and clammy skin, rapid breathing, or loss of consciousness occur, reflecting critical blood volume deficiency. Early intervention prevents complications like organ failure and shock in both dehydration and hypovolemia cases.
Dehydration Infographic
 libterm.com
libterm.com