Onychomycosis and psoriasis can both affect your nails, often causing discoloration, thickening, and distortion that may be difficult to differentiate without proper diagnosis. Effective treatment depends on accurately identifying the underlying condition since antifungal medications target onychomycosis while psoriasis requires different management strategies. Explore the rest of this article to understand key symptoms, diagnostic tips, and treatment options for these nail disorders.
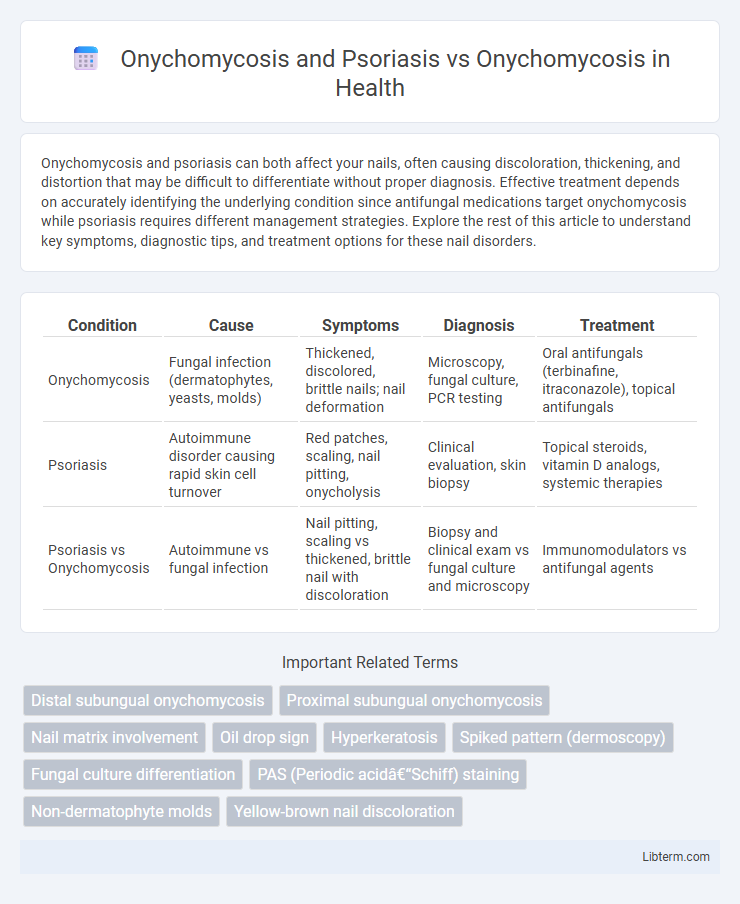
Table of Comparison
| Condition | Cause | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|
| Onychomycosis | Fungal infection (dermatophytes, yeasts, molds) | Thickened, discolored, brittle nails; nail deformation | Microscopy, fungal culture, PCR testing | Oral antifungals (terbinafine, itraconazole), topical antifungals |
| Psoriasis | Autoimmune disorder causing rapid skin cell turnover | Red patches, scaling, nail pitting, onycholysis | Clinical evaluation, skin biopsy | Topical steroids, vitamin D analogs, systemic therapies |
| Psoriasis vs Onychomycosis | Autoimmune vs fungal infection | Nail pitting, scaling vs thickened, brittle nail with discoloration | Biopsy and clinical exam vs fungal culture and microscopy | Immunomodulators vs antifungal agents |
Understanding Onychomycosis: Causes and Symptoms
Onychomycosis, a fungal infection of the nails, is characterized by thickened, discolored, and brittle nails caused primarily by dermatophytes, yeasts, or non-dermatophyte molds. Psoriasis can mimic or coexist with onychomycosis, complicating accurate diagnosis due to similar nail changes such as pitting, onycholysis, and subungual hyperkeratosis. Understanding the distinct clinical and mycological features is crucial for effective treatment, as onychomycosis requires antifungal therapy while psoriatic nail changes respond better to immunomodulators.
What is Psoriasis? Nail Involvement Explained
Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells leading to scaling and inflammation, often affecting the scalp, elbows, and knees. Nail involvement occurs in up to 50% of psoriasis patients, manifesting as pitting, discoloration, thickening, and onycholysis, which can resemble onychomycosis. Differentiating psoriasis-related nail changes from onychomycosis is crucial due to overlapping symptoms but requires distinct treatment approaches, as psoriasis results from immune dysregulation, while onychomycosis is a fungal infection.
Nail Changes in Onychomycosis vs Psoriasis
Nail changes in onychomycosis typically include thickening, discoloration (yellow, brown, or white), subungual debris, and onycholysis, which result from fungal invasion of the nail plate and bed. In contrast, psoriasis-related nail changes involve pitting, oil-drop discoloration, onycholysis, and subungual hyperkeratosis, reflecting underlying epidermal inflammation and abnormal keratinocyte proliferation. Distinguishing these conditions is crucial for effective treatment, as onychomycosis requires antifungal therapy while psoriatic nail disease often responds to immunomodulatory treatments.
Risk Factors: Who is Affected Most?
Onychomycosis primarily affects adults over 50, individuals with diabetes, immunocompromised patients, and those with frequent nail trauma or moisture exposure, increasing fungal infection susceptibility. Psoriasis-related onychomycosis risk is higher in patients with severe nail psoriasis due to nail dystrophy and impaired nail barrier function. Both conditions show elevated prevalence in men and individuals with peripheral vascular disease, but psoriasis alters the nail environment, facilitating fungal colonization compared to onychomycosis alone.
Diagnostic Challenges: Differentiating Onychomycosis and Psoriatic Nails
Onychomycosis and psoriatic nails often present overlapping clinical features such as nail discoloration, thickening, and subungual debris, complicating accurate diagnosis. Distinguishing between fungal infection and psoriasis requires careful evaluation using direct microscopy, fungal cultures, and histopathological examination to confirm the presence of dermatophytes or yeast. Accurate differentiation is critical for guiding effective treatment strategies, as antifungal therapy is essential for onychomycosis, whereas psoriasis may require immunomodulatory agents.
Clinical Features: Key Similarities and Differences
Onychomycosis and psoriasis both affect the nails, causing discoloration, thickening, and onycholysis, but onychomycosis typically presents with subungual hyperkeratosis and yellow-white fungal debris, whereas psoriatic nails often exhibit pitting, oil spots, and salmon patches. Nail involvement in psoriasis is frequently accompanied by skin lesions and joint symptoms, whereas onychomycosis is isolated to fungal infection without systemic manifestations. Accurate differentiation relies on clinical examination supported by mycological culture or histopathology to identify fungal elements in onychomycosis versus psoriatic changes in nail matrix or bed.
Laboratory Tests for Accurate Diagnosis
Laboratory tests such as KOH microscopy, fungal cultures, and PCR assays play a critical role in differentiating Onychomycosis from Psoriasis-related nail changes. Nail clippings examined under direct microscopy or cultured can confirm fungal presence, which is absent in Psoriasis without secondary infection. Histopathological analysis combined with clinical evaluation increases diagnostic accuracy, ensuring targeted antifungal therapy for Onychomycosis and appropriate treatment for Psoriasis.
Treatment Approaches for Onychomycosis
Treatment approaches for onychomycosis primarily include oral antifungal medications such as terbinafine and itraconazole, which target fungal pathogens effectively. In cases where onychomycosis coexists with psoriasis, clinicians may adjust treatment protocols to address both conditions, often integrating topical corticosteroids or vitamin D analogs alongside antifungal agents to manage inflammation and infection. Laser therapy and photodynamic therapy serve as adjunctive treatments, enhancing antifungal efficacy while minimizing adverse effects in resistant or complex cases.
Managing Psoriatic Nail Disease: Strategies and Options
Managing psoriatic nail disease involves targeted therapies such as topical corticosteroids, vitamin D analogs, and systemic treatments like biologics to reduce inflammation and nail dystrophy. Differential diagnosis of onychomycosis versus psoriatic nail changes is crucial since fungal infections require antifungal agents, whereas psoriatic nails benefit from immunomodulatory approaches. Combining clinical examination, dermoscopy, and mycological tests ensures accurate diagnosis and effective management tailored to psoriatic nail symptoms or concomitant onychomycosis.
Prognosis and Prevention: Best Practices for Nail Health
Onychomycosis combined with psoriasis complicates prognosis due to immune dysregulation and increased nail matrix vulnerability, often leading to persistent fungal infections and nail deformities compared to onychomycosis alone. Effective prevention includes rigorous nail hygiene, antifungal treatments tailored to fungal species, and managing psoriasis with systemic or topical therapies to reduce nail bed inflammation and improve treatment outcomes. Regular dermatological assessments and avoiding nail trauma are essential best practices to maintain optimal nail health and prevent recurrence in both conditions.
Onychomycosis and Psoriasis Infographic
 libterm.com
libterm.com