Maintaining optimal glycemic control is essential for preventing complications in individuals with diabetes by keeping blood sugar levels within a target range. Effective strategies include monitoring glucose regularly, adhering to prescribed medications, and adopting a balanced diet coupled with consistent physical activity. Discover how you can improve your glycemic control and enhance your overall health by exploring the rest of this article.
Table of Comparison
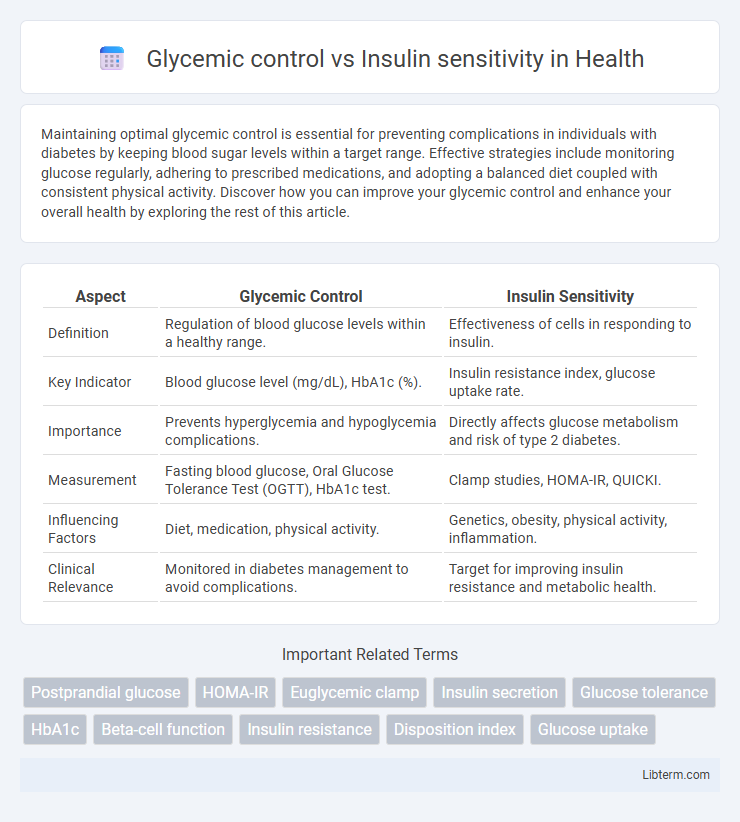
| Aspect | Glycemic Control | Insulin Sensitivity |
|---|---|---|
| Definition | Regulation of blood glucose levels within a healthy range. | Effectiveness of cells in responding to insulin. |
| Key Indicator | Blood glucose level (mg/dL), HbA1c (%). | Insulin resistance index, glucose uptake rate. |
| Importance | Prevents hyperglycemia and hypoglycemia complications. | Directly affects glucose metabolism and risk of type 2 diabetes. |
| Measurement | Fasting blood glucose, Oral Glucose Tolerance Test (OGTT), HbA1c test. | Clamp studies, HOMA-IR, QUICKI. |
| Influencing Factors | Diet, medication, physical activity. | Genetics, obesity, physical activity, inflammation. |
| Clinical Relevance | Monitored in diabetes management to avoid complications. | Target for improving insulin resistance and metabolic health. |
Understanding Glycemic Control
Glycemic control refers to the maintenance of blood glucose levels within a target range to prevent hyperglycemia and hypoglycemia in individuals with diabetes or metabolic disorders. Effective glycemic control is achieved by balancing insulin secretion, glucose uptake by tissues, and hepatic glucose production, which directly impacts long-term complications such as neuropathy and cardiovascular disease. Monitoring parameters like HbA1c, fasting blood glucose, and postprandial glucose helps evaluate glycemic control and tailor treatment plans to improve patient outcomes.
Defining Insulin Sensitivity
Insulin sensitivity refers to how effectively the body's cells respond to insulin, facilitating glucose uptake from the bloodstream into tissues like muscle and fat. High insulin sensitivity allows for efficient blood sugar regulation, minimizing the risk of hyperglycemia and type 2 diabetes. Measuring insulin sensitivity helps assess metabolic health and the body's ability to maintain glycemic control.
Key Differences Between Glycemic Control and Insulin Sensitivity
Glycemic control refers to the regulation of blood glucose levels through mechanisms involving insulin secretion and glucose uptake, often monitored by metrics like HbA1c and fasting blood glucose. Insulin sensitivity measures how effectively cells respond to insulin, influencing glucose absorption and metabolism at the cellular level, commonly assessed through tests like the HOMA-IR or the glucose tolerance test. The key difference lies in glycemic control being a broader outcome of multiple physiological processes managing blood sugar, while insulin sensitivity specifically reflects cellular responsiveness to insulin's action.
Mechanisms Underlying Glycemic Control
Glycemic control is primarily regulated by the coordinated action of insulin secretion from pancreatic beta-cells and insulin sensitivity of peripheral tissues, particularly muscle and adipose tissue. Insulin facilitates glucose uptake by promoting GLUT4 translocation to the cell membrane, while also suppressing hepatic gluconeogenesis to maintain euglycemia. Dysregulation in these mechanisms, such as impaired insulin signaling or beta-cell dysfunction, leads to hyperglycemia and contributes to the pathogenesis of type 2 diabetes.
Factors Influencing Insulin Sensitivity
Insulin sensitivity is primarily influenced by factors such as physical activity, body composition, and dietary habits, with regular exercise enhancing glucose uptake by muscle cells. Obesity, particularly visceral fat accumulation, impairs insulin signaling pathways, reducing insulin sensitivity and increasing the risk of type 2 diabetes. Genetic predisposition, inflammation, and hormonal imbalances also play critical roles in modulating an individual's response to insulin and overall glycemic control.
Clinical Significance of Glycemic Control in Diabetes
Glycemic control, measured by HbA1c levels, is crucial in diabetes management to prevent microvascular complications such as retinopathy, nephropathy, and neuropathy. Improved glycemic control reduces the risk of cardiovascular events and hospitalizations in both type 1 and type 2 diabetes populations. Insulin sensitivity influences glucose uptake, but clinical outcomes strongly correlate with maintaining target glycemic levels to minimize long-term complications.
Assessing Insulin Sensitivity: Common Methods
Assessing insulin sensitivity is crucial for understanding glucose metabolism and managing conditions like type 2 diabetes. Common methods include the hyperinsulinemic-euglycemic clamp, considered the gold standard, and the frequently sampled intravenous glucose tolerance test (FSIVGTT), which provides dynamic insulin and glucose response data. Simpler alternatives like the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) use fasting glucose and insulin levels to estimate insulin sensitivity in clinical settings.
Diet and Lifestyle Impact on Both Parameters
Diet rich in whole grains, fiber, and low-glycemic index foods enhances glycemic control by stabilizing blood sugar levels and reducing insulin spikes. Regular physical activity improves insulin sensitivity by increasing glucose uptake in muscle cells, facilitating better metabolic responses. Weight management through balanced nutrition and exercise plays a critical role in optimizing both glycemic control and insulin sensitivity, reducing the risk of type 2 diabetes.
Improving Glycemic Control and Insulin Sensitivity
Improving glycemic control involves maintaining blood glucose levels within a target range to prevent complications associated with diabetes, often achieved through diet, exercise, and medication. Enhancing insulin sensitivity enables cells to respond effectively to insulin, reducing blood sugar levels and lowering the risk of type 2 diabetes. Strategies such as regular physical activity, weight management, and consumption of low-glycemic index foods play a critical role in optimizing both glycemic control and insulin sensitivity.
Integrating Glycemic Control & Insulin Sensitivity in Diabetes Management
Integrating glycemic control and insulin sensitivity is crucial for effective diabetes management, as optimizing both parameters reduces blood glucose fluctuations and enhances overall metabolic health. Targeted therapies, including insulin sensitizers like metformin and lifestyle interventions such as aerobic exercise, improve insulin action while maintaining stable glycemic levels. Continuous glucose monitoring combined with personalized treatment plans allows for precise adjustments that address insulin resistance and minimize hyperglycemia risks.
Glycemic control Infographic
 libterm.com
libterm.com