Pseudo-obstruction mimics symptoms of a mechanical bowel obstruction without an actual physical blockage, causing abdominal pain, bloating, and severe constipation. This condition disrupts normal intestinal motility, often requiring specialized diagnosis and management strategies. Explore the rest of the article to understand the causes, symptoms, and treatment options for pseudo-obstruction.
Table of Comparison
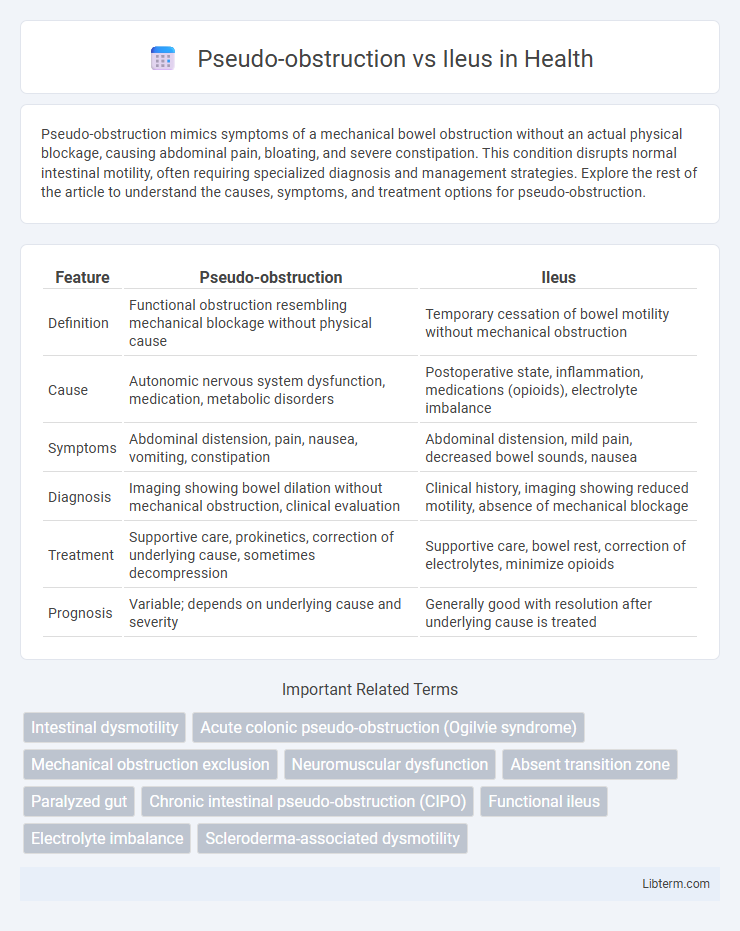
| Feature | Pseudo-obstruction | Ileus |
|---|---|---|
| Definition | Functional obstruction resembling mechanical blockage without physical cause | Temporary cessation of bowel motility without mechanical obstruction |
| Cause | Autonomic nervous system dysfunction, medication, metabolic disorders | Postoperative state, inflammation, medications (opioids), electrolyte imbalance |
| Symptoms | Abdominal distension, pain, nausea, vomiting, constipation | Abdominal distension, mild pain, decreased bowel sounds, nausea |
| Diagnosis | Imaging showing bowel dilation without mechanical obstruction, clinical evaluation | Clinical history, imaging showing reduced motility, absence of mechanical blockage |
| Treatment | Supportive care, prokinetics, correction of underlying cause, sometimes decompression | Supportive care, bowel rest, correction of electrolytes, minimize opioids |
| Prognosis | Variable; depends on underlying cause and severity | Generally good with resolution after underlying cause is treated |
Understanding Pseudo-obstruction and Ileus
Pseudo-obstruction mimics mechanical bowel obstruction without a physical blockage, caused by nerve or muscle dysfunction disrupting normal intestinal motility. Ileus, on the other hand, is a temporary impairment of bowel motility often triggered by surgery, infection, or medications, leading to a functional obstruction. Accurate differentiation relies on clinical evaluation, imaging studies like abdominal X-rays or CT scans, and exclusion of mechanical causes.
Key Differences Between Pseudo-obstruction and Ileus
Pseudo-obstruction is characterized by symptoms resembling intestinal blockage without any physical obstruction, primarily caused by nerve or muscle dysfunction in the gastrointestinal tract. Ileus involves temporary cessation of bowel motility, often following surgery, infection, or medication use, leading to accumulation of intestinal contents and gas. Key differences include the underlying mechanisms--pseudo-obstruction results from chronic autonomic nervous system impairment, whereas ileus is typically acute and related to external factors or systemic illness.
Etiology and Risk Factors
Pseudo-obstruction typically arises from autonomic nervous system dysfunction or underlying neurological disorders such as Parkinson's disease, diabetes mellitus, and multiple sclerosis. Ileus commonly results from postoperative abdominal surgery, electrolyte imbalances like hypokalemia, or use of certain medications including opioids and anticholinergics. Both conditions share risk factors such as advanced age, severe infections, and systemic illnesses that impair gastrointestinal motility.
Pathophysiology of Pseudo-obstruction
Pseudo-obstruction, also known as Ogilvie's syndrome, involves impaired motility of the colon without a mechanical blockage, often caused by autonomic nervous system dysfunction or underlying conditions like infections, medications, or metabolic imbalances. The pathophysiology centers on disrupted neural regulation of colonic smooth muscle activity, leading to ineffective peristalsis and massive colonic dilatation. In contrast, ileus typically results from generalized bowel paralysis due to postoperative states, inflammation, or ischemia, with broader impairment of both small and large intestine motility.
Mechanisms Underlying Ileus
Ileus results from a disruption in normal gastrointestinal motility due to impaired neural regulation, inflammatory responses, or electrolyte imbalances affecting smooth muscle contractility. The mechanism involves inhibition of excitatory motor neurons and activation of inhibitory pathways within the enteric nervous system, leading to reduced peristalsis and bowel stasis. In contrast, pseudo-obstruction exhibits similar symptoms but is characterized by a non-mechanical cause with underlying neuropathic or myopathic abnormalities affecting intestinal motility.
Clinical Presentation and Symptoms
Pseudo-obstruction presents with symptoms mimicking mechanical bowel obstruction, including abdominal distension, pain, nausea, vomiting, and constipation, without any physical blockage on imaging or surgery. Ileus typically features generalized abdominal discomfort, decreased bowel sounds, bloating, and failure of bowel motility following surgery or infection, leading to delayed passage of gas and stool. Both conditions show signs of bowel dysfunction, but pseudo-obstruction often has intermittent symptom episodes linked to autonomic or metabolic disturbances, whereas ileus is usually continuous and related to underlying illness or surgical intervention.
Diagnostic Approaches
Diagnostic approaches for pseudo-obstruction involve radiographic imaging such as abdominal X-rays and CT scans to identify dilated bowel loops without mechanical obstruction, complemented by manometry to assess motility disorders. Ileus diagnosis relies on clinical evaluation, abdominal imaging demonstrating diffuse bowel distension with air-fluid levels, and the exclusion of mechanical causes through contrast studies or laparotomy if needed. Laboratory tests may assist in identifying underlying causes like electrolyte imbalances or infections contributing to ileus.
Imaging and Laboratory Findings
Imaging for pseudo-obstruction typically shows massive colonic dilation without a mechanical obstruction on abdominal X-rays or CT scans, whereas ileus reveals diffuse bowel gas patterns with both small and large bowel dilation and no transition point. Laboratory findings in pseudo-obstruction often demonstrate normal inflammatory markers and electrolytes, while ileus may present with elevated white blood cell count, electrolyte imbalances, and signs of underlying infection or inflammation. Radiographic contrast studies can help differentiate pseudo-obstruction by excluding mechanical causes, whereas ileus reflects bowel motility dysfunction secondary to critical illness or surgery.
Treatment Strategies
Treatment strategies for pseudo-obstruction primarily involve decompression with nasogastric or colonoscopic interventions and addressing underlying causes such as electrolyte imbalances or infections. Ileus management focuses on supportive care including bowel rest, fluid and electrolyte optimization, and minimizing the use of narcotics or other medications that impair motility. Pharmacologic agents like neostigmine are often effective in pseudo-obstruction, whereas ileus usually resolves with conservative measures and correction of precipitating factors.
Prognosis and Long-Term Outcomes
Pseudo-obstruction and ileus differ significantly in prognosis and long-term outcomes, with pseudo-obstruction often presenting a chronic, relapsing course requiring ongoing management to prevent complications such as malnutrition and bacterial overgrowth. Ileus, typically transient and self-limiting post-surgical or secondary to acute illness, generally resolves without long-term sequelae but may prolong hospitalization and increase morbidity in complex cases. Effective differentiation and appropriate treatment strategies directly impact patient recovery trajectories and reduce the risk of recurrent episodes or permanent gastrointestinal dysfunction.
Pseudo-obstruction Infographic
 libterm.com
libterm.com