Healthcare-associated infections (HAIs) pose significant risks to patient safety, occurring during the delivery of medical care in hospitals or other healthcare settings. These infections can lead to prolonged hospital stays, increased medical costs, and severe complications. Explore the article to understand how you can prevent HAIs and promote safer healthcare environments.
Table of Comparison
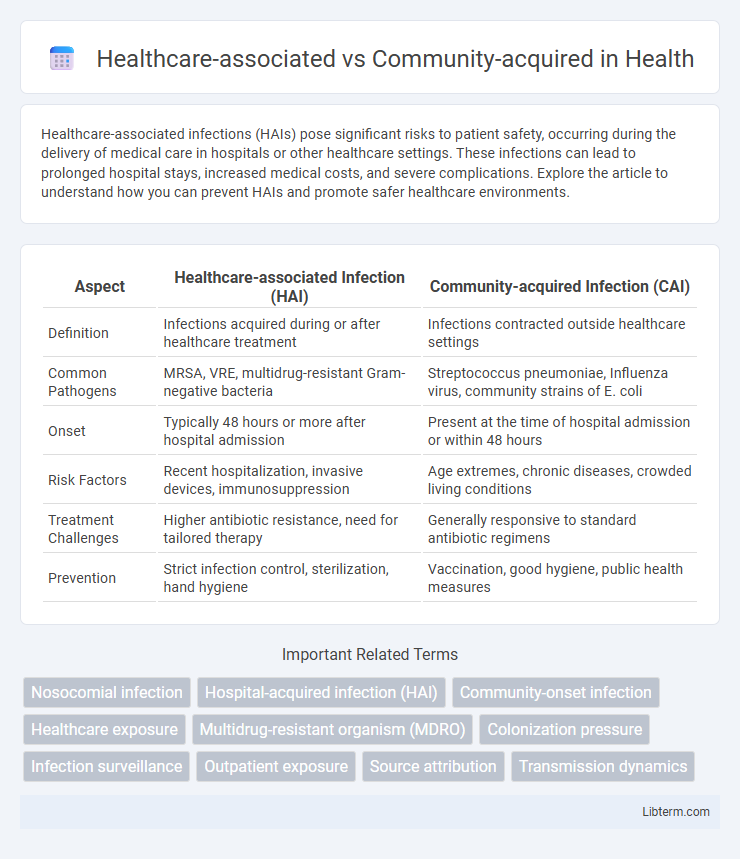
| Aspect | Healthcare-associated Infection (HAI) | Community-acquired Infection (CAI) |
|---|---|---|
| Definition | Infections acquired during or after healthcare treatment | Infections contracted outside healthcare settings |
| Common Pathogens | MRSA, VRE, multidrug-resistant Gram-negative bacteria | Streptococcus pneumoniae, Influenza virus, community strains of E. coli |
| Onset | Typically 48 hours or more after hospital admission | Present at the time of hospital admission or within 48 hours |
| Risk Factors | Recent hospitalization, invasive devices, immunosuppression | Age extremes, chronic diseases, crowded living conditions |
| Treatment Challenges | Higher antibiotic resistance, need for tailored therapy | Generally responsive to standard antibiotic regimens |
| Prevention | Strict infection control, sterilization, hand hygiene | Vaccination, good hygiene, public health measures |
Introduction to Healthcare-Associated and Community-Acquired Infections
Healthcare-associated infections (HAIs) occur in patients receiving treatment within healthcare settings, including hospitals, clinics, and long-term care facilities, often involving multidrug-resistant organisms. Community-acquired infections (CAIs) develop outside healthcare environments, typically in healthy individuals, and are usually caused by common pathogens sensitive to standard treatments. Understanding the distinction between HAIs and CAIs is crucial for implementing targeted infection control measures and appropriate antimicrobial therapies.
Key Definitions and Distinctions
Healthcare-associated infections (HAIs) occur in patients during or after receiving treatment in healthcare settings, often linked to invasive procedures or devices, and are frequently caused by antibiotic-resistant pathogens. Community-acquired infections develop outside healthcare facilities, affecting individuals with no recent exposure to medical environments, typically involving common pathogens with predictable resistance patterns. Distinguishing HAIs from community-acquired infections is crucial for epidemiology, guiding appropriate antimicrobial therapy and infection control strategies.
Common Pathogens: A Comparative Overview
Healthcare-associated infections (HAIs) commonly involve pathogens such as methicillin-resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa, and Clostridioides difficile, reflecting antibiotic resistance and hospital environment exposure. In contrast, community-acquired infections are frequently caused by pathogens like Streptococcus pneumoniae, Haemophilus influenzae, and non-resistant strains of Escherichia coli, which circulate more widely outside healthcare settings. Understanding these differences in pathogen profiles is crucial for selecting appropriate empiric antibiotic therapy and implementing targeted infection control measures.
Risk Factors in Healthcare Settings
Risk factors for healthcare-associated infections (HAIs) include prolonged hospitalization, invasive procedures such as catheterization or surgery, and the use of immunosuppressive therapies. Patients in intensive care units (ICUs) or with weakened immune systems face higher susceptibility due to increased exposure to multidrug-resistant organisms. Strict adherence to infection control protocols and environmental sanitation is critical in minimizing these risks within healthcare settings.
Community Exposure and Sources of Infection
Community-acquired infections originate from exposure to pathogens present in everyday environments such as public spaces, schools, and workplaces, where individuals come into contact with infected people or contaminated surfaces. Common sources include respiratory droplets, contaminated food, water, and direct person-to-person transmission, often involving viruses like influenza or bacteria like Streptococcus pneumoniae. Understanding these exposure pathways helps in designing prevention strategies targeting hygiene, vaccination, and public health awareness outside healthcare settings.
Clinical Presentation Differences
Healthcare-associated infections often present with multidrug-resistant pathogens and more severe clinical symptoms due to patients' underlying comorbidities and frequent healthcare exposures. Community-acquired infections typically involve common pathogens with a rapid onset of symptoms in otherwise healthy individuals, manifesting as localized or systemic signs depending on the infection type. Recognizing these clinical presentation differences is critical for guiding empirical antibiotic therapy and infection control measures.
Diagnostic Approaches for Accurate Identification
Healthcare-associated infections often require advanced diagnostic tools such as molecular assays and biomarker analysis to distinguish from community-acquired cases due to varied pathogen profiles and antibiotic resistance patterns. Community-acquired infections are typically identified using standard culture methods and rapid antigen tests, reflecting common pathogens with predictable sensitivities. Accurate identification relies on integrating patient history, clinical presentation, and tailored diagnostic tests to guide targeted therapy and infection control measures effectively.
Treatment Strategies and Challenges
Treatment strategies for healthcare-associated infections often involve broad-spectrum antibiotics due to multidrug-resistant organisms, posing significant challenges in selecting effective therapies. Community-acquired infections generally respond to standard antibiotic regimens but require careful differentiation to avoid overtreatment or misuse. The complexity of resistance patterns in healthcare settings necessitates ongoing surveillance and tailored antimicrobial stewardship programs to optimize patient outcomes.
Prevention and Control Measures
Healthcare-associated infections require stringent prevention and control measures including strict hand hygiene, use of personal protective equipment, and environmental cleaning protocols in medical settings. Community-acquired infections are managed through vaccination programs, public health education, and early detection strategies to reduce transmission. Both settings benefit from antimicrobial stewardship to prevent resistance and improve patient outcomes.
Impact on Public Health and Healthcare Systems
Healthcare-associated infections (HAIs) significantly burden healthcare systems by increasing hospital stays, treatment costs, and antimicrobial resistance rates, which complicate patient management and resource allocation. Community-acquired infections often present broader public health challenges due to their potential for rapid spread and large-scale outbreaks, necessitating extensive surveillance and preventive measures. Effective differentiation and management of these infections are crucial to optimizing healthcare resources and mitigating public health risks.
Healthcare-associated Infographic
 libterm.com
libterm.com