Hyponatremia occurs when your blood sodium levels fall below normal, disrupting cellular functions and causing symptoms like confusion, headache, and fatigue. This electrolyte imbalance often results from excessive fluid intake, certain medications, or underlying medical conditions such as heart failure or kidney disease. Learn more about its causes, symptoms, and effective treatment options to manage hyponatremia in the following article.
Table of Comparison
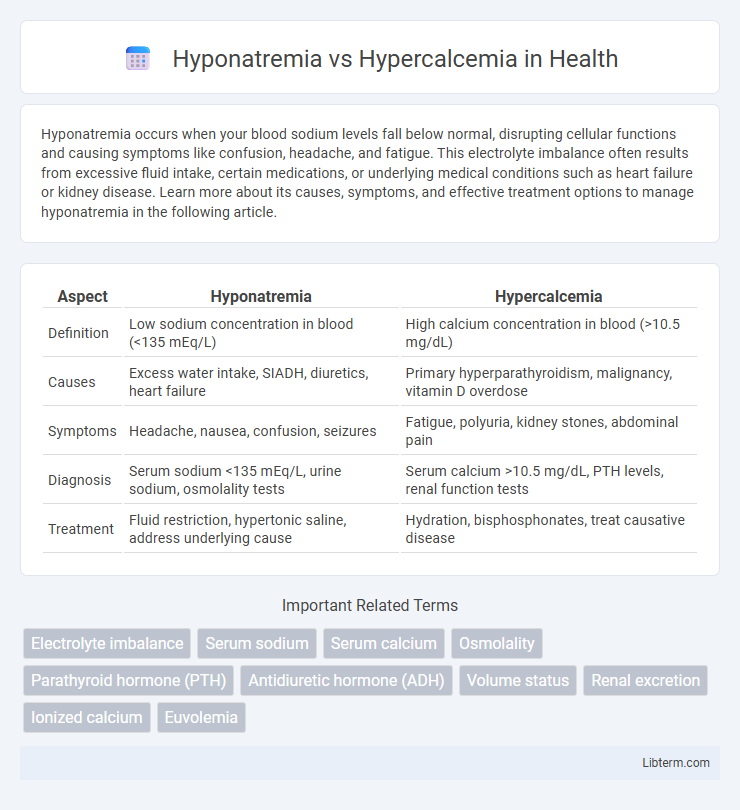
| Aspect | Hyponatremia | Hypercalcemia |
|---|---|---|
| Definition | Low sodium concentration in blood (<135 mEq/L) | High calcium concentration in blood (>10.5 mg/dL) |
| Causes | Excess water intake, SIADH, diuretics, heart failure | Primary hyperparathyroidism, malignancy, vitamin D overdose |
| Symptoms | Headache, nausea, confusion, seizures | Fatigue, polyuria, kidney stones, abdominal pain |
| Diagnosis | Serum sodium <135 mEq/L, urine sodium, osmolality tests | Serum calcium >10.5 mg/dL, PTH levels, renal function tests |
| Treatment | Fluid restriction, hypertonic saline, address underlying cause | Hydration, bisphosphonates, treat causative disease |
Introduction to Hyponatremia and Hypercalcemia
Hyponatremia is a common electrolyte disorder characterized by a serum sodium concentration below 135 mmol/L, often caused by excessive water retention or sodium loss, leading to neurological symptoms such as confusion and seizures. Hypercalcemia, defined by serum calcium levels exceeding 10.5 mg/dL, results from increased bone resorption, excessive intestinal absorption, or impaired renal excretion, frequently associated with hyperparathyroidism or malignancy. Both conditions require prompt diagnosis and management due to their potential to cause significant morbidity, impacting electrolyte balance and cellular function.
Pathophysiology: Sodium vs Calcium Imbalance
Hyponatremia occurs due to an imbalance in sodium levels often caused by excessive water retention or sodium loss, leading to cellular swelling and impaired nerve and muscle function. Hypercalcemia stems from elevated calcium levels, usually resulting from increased bone resorption, enhanced gastrointestinal absorption, or reduced renal excretion, causing neuromuscular excitability and altered cardiac conduction. Both disturbances disrupt electrolyte homeostasis but affect cellular activity and fluid balance through distinct mechanisms involving sodium and calcium ions.
Causes of Hyponatremia
Hyponatremia primarily results from excessive water intake, syndrome of inappropriate antidiuretic hormone secretion (SIADH), heart failure, liver cirrhosis, and certain diuretics that disrupt sodium balance. Other causes include adrenal insufficiency, hypothyroidism, and conditions causing renal sodium loss such as Addison's disease. Understanding these root causes is crucial for accurate diagnosis and effective management of low serum sodium levels.
Causes of Hypercalcemia
Hypercalcemia primarily results from hyperparathyroidism, malignancies such as lung or breast cancer, and excessive vitamin D intake. Other causes include granulomatous diseases like sarcoidosis, certain medications like thiazide diuretics, and prolonged immobilization. Identifying these causes is crucial for effective treatment and management of elevated serum calcium levels.
Clinical Manifestations: Symptoms and Signs
Hyponatremia commonly presents with neurological symptoms such as headache, confusion, nausea, and seizures due to cerebral edema from low sodium levels. Hypercalcemia often manifests with fatigue, muscle weakness, polyuria, and neuropsychiatric disturbances like depression or cognitive dysfunction because of elevated calcium impairing neuronal activity. Both electrolyte imbalances require timely recognition of their distinct clinical signs to prevent severe complications such as coma in hyponatremia and cardiac arrhythmias in hypercalcemia.
Diagnostic Approaches and Laboratory Findings
Hyponatremia diagnosis involves serum sodium measurement below 135 mEq/L, with further evaluation of serum osmolality, urine sodium, and urine osmolality to determine underlying causes like SIADH or volume depletion. Hypercalcemia diagnosis requires total serum calcium or ionized calcium assessment above 10.5 mg/dL, alongside parathyroid hormone (PTH) testing to differentiate primary hyperparathyroidism from malignancy-related hypercalcemia. Additional laboratory findings include renal function tests and vitamin D levels for hypercalcemia, and assessment of thyroid and adrenal function in hyponatremia cases.
Acute vs Chronic Presentations
Hyponatremia presents acutely with neurological symptoms such as confusion, seizures, and coma due to cerebral edema, while chronic hyponatremia tends to cause milder cognitive impairment and gait disturbances. Acute hypercalcemia often manifests with severe symptoms like dehydration, renal failure, and altered mental status, whereas chronic hypercalcemia typically results in bone pain, nephrolithiasis, and muscle weakness. Distinguishing acute from chronic forms in both disorders is crucial for tailored management and preventing long-term complications.
Treatment Strategies for Hyponatremia
Treatment strategies for hyponatremia depend on the severity and underlying cause, with acute symptomatic hyponatremia often requiring rapid correction using hypertonic saline (3% NaCl) under careful monitoring to prevent osmotic demyelination syndrome. For chronic hyponatremia, fluid restriction and addressing the underlying cause, such as syndrome of inappropriate antidiuretic hormone secretion (SIADH), are primary approaches, along with potential use of vasopressin receptor antagonists like tolvaptan. In contrast, hypercalcemia treatment typically involves aggressive hydration, bisphosphonates, and addressing the underlying malignancy or hyperparathyroidism, highlighting distinct therapeutic pathways between these electrolyte disturbances.
Management Options for Hypercalcemia
Management options for hypercalcemia primarily include intravenous hydration with isotonic saline to enhance renal calcium excretion and administration of bisphosphonates like zoledronic acid or pamidronate to inhibit bone resorption. Calcitonin provides a rapid but short-term reduction in serum calcium levels, useful in acute settings, while corticosteroids are effective in cases related to vitamin D intoxication or certain malignancies. In severe or refractory cases, dialysis may be necessary, particularly when renal function is compromised.
Prognosis and Long-term Complications
Hyponatremia prognosis depends on severity and underlying cause, with acute cases potentially causing cerebral edema and chronic cases linked to increased morbidity and mortality. Hypercalcemia prognosis varies, often related to malignancy or parathyroid disorders, with severe cases risking nephrocalcinosis, kidney stones, and cardiac arrhythmias. Long-term complications of hyponatremia include persistent cognitive impairment and falls, while hypercalcemia can lead to chronic kidney disease and osteoporosis.
Hyponatremia Infographic
 libterm.com
libterm.com