A subarachnoid hemorrhage occurs when there is bleeding in the space between the brain and the tissues covering the brain, often resulting from a ruptured aneurysm. This condition can cause sudden, severe headaches, neurological deficits, and requires immediate medical attention to prevent serious complications or death. Discover the essential symptoms, causes, and treatment options to protect your health in the full article.
Table of Comparison
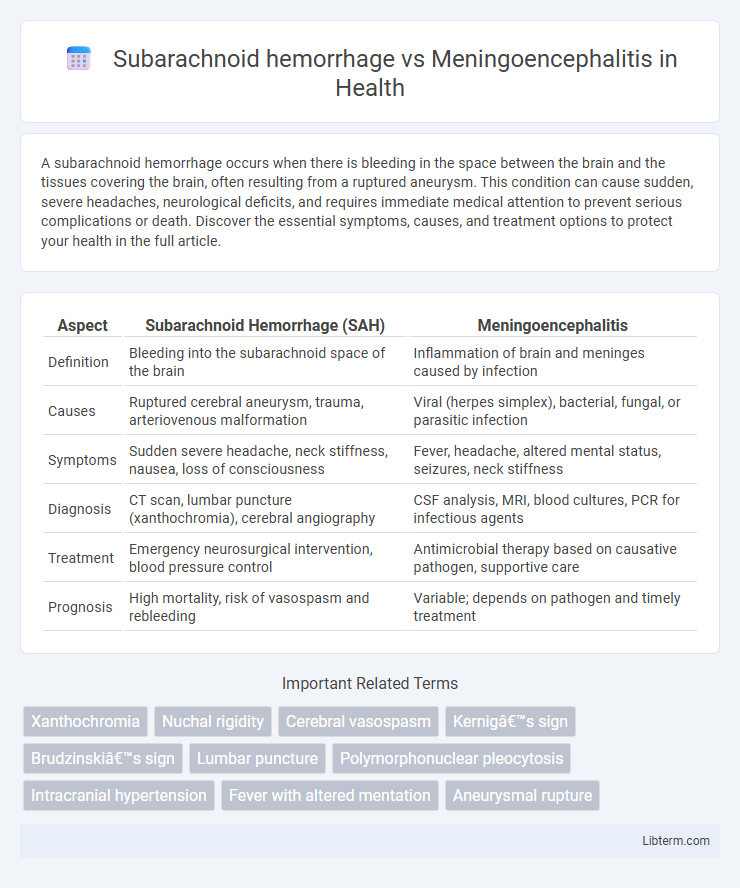
| Aspect | Subarachnoid Hemorrhage (SAH) | Meningoencephalitis |
|---|---|---|
| Definition | Bleeding into the subarachnoid space of the brain | Inflammation of brain and meninges caused by infection |
| Causes | Ruptured cerebral aneurysm, trauma, arteriovenous malformation | Viral (herpes simplex), bacterial, fungal, or parasitic infection |
| Symptoms | Sudden severe headache, neck stiffness, nausea, loss of consciousness | Fever, headache, altered mental status, seizures, neck stiffness |
| Diagnosis | CT scan, lumbar puncture (xanthochromia), cerebral angiography | CSF analysis, MRI, blood cultures, PCR for infectious agents |
| Treatment | Emergency neurosurgical intervention, blood pressure control | Antimicrobial therapy based on causative pathogen, supportive care |
| Prognosis | High mortality, risk of vasospasm and rebleeding | Variable; depends on pathogen and timely treatment |
Introduction: Subarachnoid Hemorrhage vs Meningoencephalitis
Subarachnoid hemorrhage (SAH) is a critical condition characterized by bleeding into the subarachnoid space, often caused by ruptured cerebral aneurysms, leading to sudden severe headache and neurological deficits. Meningoencephalitis involves inflammation of both the meninges and brain parenchyma, typically resulting from viral or bacterial infections, presenting with fever, headache, altered mental status, and seizures. Differentiating these conditions relies on clinical presentation, neuroimaging, and cerebrospinal fluid analysis to guide timely and appropriate management.
Definition and Basic Pathophysiology
Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space, usually caused by a ruptured cerebral aneurysm, leading to increased intracranial pressure and impaired cerebrospinal fluid dynamics. Meningoencephalitis is the inflammation of the brain parenchyma and meninges, often resulting from viral or bacterial infections, causing neuronal damage and blood-brain barrier disruption. Both conditions involve critical neurological dysfunction but differ fundamentally in etiology with SAH being hemorrhagic and meningoencephalitis primarily inflammatory and infectious.
Epidemiology and Risk Factors
Subarachnoid hemorrhage (SAH) primarily affects adults aged 40-60, with an incidence of approximately 9 per 100,000 annually, and risk factors include hypertension, smoking, and aneurysm rupture. Meningoencephalitis, often caused by viral or bacterial infections, has a variable incidence globally, with higher rates in immunocompromised individuals and those exposed to endemic pathogens. Epidemiological patterns reveal that SAH is more common in populations with a history of cerebrovascular disease, while meningoencephalitis incidence correlates with infectious outbreaks and seasonal variations.
Etiology: Causes and Triggers
Subarachnoid hemorrhage primarily results from the rupture of cerebral aneurysms or arteriovenous malformations, often triggered by hypertension or head trauma. In contrast, meningoencephalitis is caused by infectious agents such as viruses (Herpes simplex virus, enteroviruses), bacteria (Neisseria meningitidis, Streptococcus pneumoniae), or autoimmune inflammatory processes. While SAH is a vascular event involving bleeding into the subarachnoid space, meningoencephalitis is characterized by inflammation of both the meninges and brain parenchyma due to infectious or immune-mediated triggers.
Clinical Presentation: Signs and Symptoms
Subarachnoid hemorrhage typically presents with a sudden, severe "thunderclap" headache, often described as the worst headache of the patient's life, accompanied by neck stiffness, photophobia, and sometimes loss of consciousness. Meningoencephalitis manifests with fever, headache, altered mental status, focal neurological deficits, and signs of meningeal irritation such as nuchal rigidity. Both conditions can present with headache and altered consciousness, but the rapid onset and severity of headache are more characteristic of subarachnoid hemorrhage, while fever and progressive neurological decline are more indicative of meningoencephalitis.
Diagnostic Criteria and Key Investigations
Subarachnoid hemorrhage is diagnosed primarily through non-contrast CT scan revealing blood in the subarachnoid space, with lumbar puncture confirming xanthochromia if the CT is negative. Meningoencephalitis diagnosis relies on cerebrospinal fluid analysis showing elevated white blood cells, increased protein, and decreased glucose, alongside MRI highlighting inflammatory changes in brain parenchyma and meninges. Both conditions require urgent neuroimaging and CSF studies, but subarachnoid hemorrhage emphasizes vascular abnormalities, while meningoencephalitis focuses on infectious and inflammatory markers.
Neuroimaging Findings and Laboratory Tests
Subarachnoid hemorrhage (SAH) neuroimaging typically reveals hyperdense blood within the subarachnoid space on non-contrast CT, with CT angiography often identifying aneurysms or vascular malformations, while cerebrospinal fluid (CSF) analysis shows xanthochromia and elevated red blood cells without significant pleocytosis. Meningoencephalitis imaging commonly presents with MRI findings of hyperintense lesions on T2-weighted or FLAIR sequences, particularly in the temporal lobes for herpes simplex virus, combined with CSF analysis indicating pleocytosis, elevated protein, and positive polymerase chain reaction (PCR) for infectious agents. Differentiating SAH from meningoencephalitis relies on the absence of infectious markers and presence of blood products in CSF for SAH versus inflammatory and infectious biomarkers in meningoencephalitis.
Treatment Approaches and Management Strategies
Subarachnoid hemorrhage treatment prioritizes urgent neurosurgical intervention, including aneurysm clipping or endovascular coiling, alongside aggressive blood pressure control and prevention of vasospasm using calcium channel blockers like nimodipine. Meningoencephalitis management involves timely administration of empirical intravenous antimicrobials tailored to likely pathogens, corticosteroids to reduce brain inflammation, and supportive care such as seizure control and intracranial pressure monitoring. Both conditions require critical monitoring in intensive care units to manage complications and optimize patient outcomes.
Prognosis and Potential Complications
Subarachnoid hemorrhage (SAH) typically has a guarded prognosis due to risks of vasospasm, rebleeding, and hydrocephalus, which can lead to permanent neurological deficits or death. Meningoencephalitis prognosis varies widely depending on the causative pathogen, with bacterial forms often causing severe complications like brain abscess, seizures, and long-term cognitive impairment. Both conditions require prompt diagnosis and treatment to minimize complications such as increased intracranial pressure and secondary brain injury.
Prevention, Follow-Up, and Patient Education
Prevention of subarachnoid hemorrhage primarily involves controlling hypertension, avoiding smoking, and managing aneurysms, while meningoencephalitis prevention focuses on vaccinations, mosquito control, and avoiding contact with infected individuals. Follow-up for subarachnoid hemorrhage includes monitoring for vasospasm, neurological deficits, and hydrocephalus, whereas meningoencephalitis follow-up requires surveillance for cognitive impairment, seizures, and residual neurological symptoms. Patient education must emphasize recognizing early symptoms, adherence to treatment regimens, and lifestyle modifications to reduce recurrence risk in subarachnoid hemorrhage and promoting hygiene and timely medical consultation to prevent and manage meningoencephalitis effectively.
Subarachnoid hemorrhage Infographic
 libterm.com
libterm.com