Cholecystitis causes inflammation of the gallbladder, often resulting in severe abdominal pain and digestive issues. Timely diagnosis through ultrasound and blood tests is crucial to prevent complications such as gallbladder rupture or infection spread. Learn more about symptoms, treatment options, and when to seek medical care to protect your health.
Table of Comparison
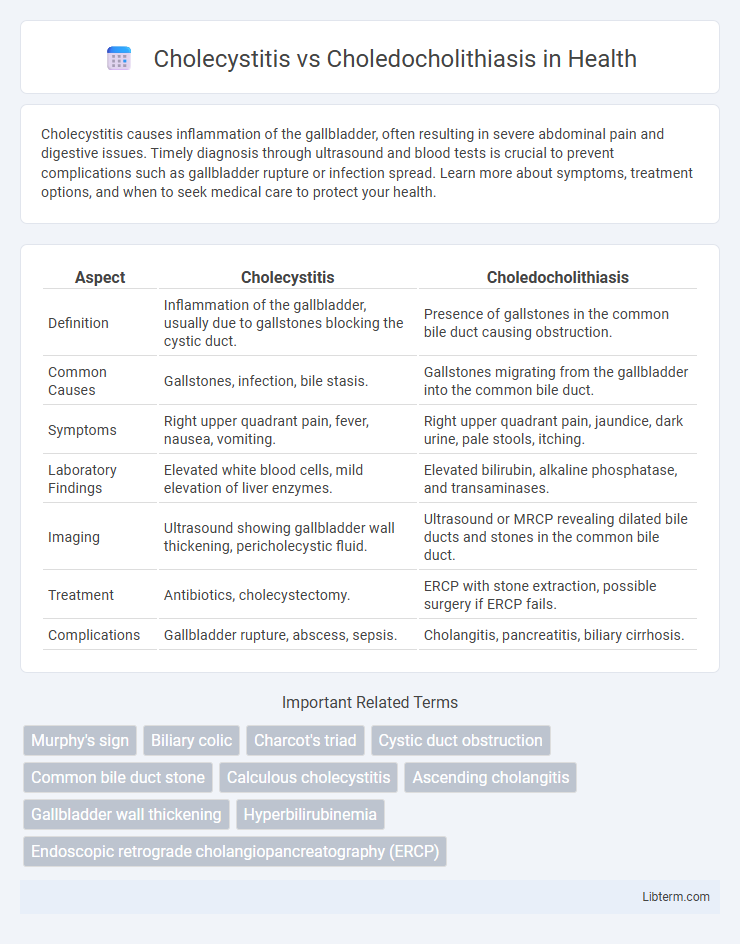
| Aspect | Cholecystitis | Choledocholithiasis |
|---|---|---|
| Definition | Inflammation of the gallbladder, usually due to gallstones blocking the cystic duct. | Presence of gallstones in the common bile duct causing obstruction. |
| Common Causes | Gallstones, infection, bile stasis. | Gallstones migrating from the gallbladder into the common bile duct. |
| Symptoms | Right upper quadrant pain, fever, nausea, vomiting. | Right upper quadrant pain, jaundice, dark urine, pale stools, itching. |
| Laboratory Findings | Elevated white blood cells, mild elevation of liver enzymes. | Elevated bilirubin, alkaline phosphatase, and transaminases. |
| Imaging | Ultrasound showing gallbladder wall thickening, pericholecystic fluid. | Ultrasound or MRCP revealing dilated bile ducts and stones in the common bile duct. |
| Treatment | Antibiotics, cholecystectomy. | ERCP with stone extraction, possible surgery if ERCP fails. |
| Complications | Gallbladder rupture, abscess, sepsis. | Cholangitis, pancreatitis, biliary cirrhosis. |
Introduction to Cholecystitis and Choledocholithiasis
Cholecystitis is the inflammation of the gallbladder, typically caused by gallstones obstructing the cystic duct, resulting in pain and infection. Choledocholithiasis involves the presence of gallstones in the common bile duct, leading to bile flow obstruction and potential complications like jaundice and pancreatitis. Both conditions require timely diagnosis and management to prevent severe biliary tract complications.
Understanding Gallbladder Anatomy and Function
The gallbladder, a small pear-shaped organ beneath the liver, stores and concentrates bile essential for fat digestion. Cholecystitis involves inflammation of the gallbladder, often due to gallstones obstructing the cystic duct, while choledocholithiasis refers to gallstones lodged in the common bile duct, impacting bile flow to the intestine. Recognizing the anatomical differences between the cystic duct and common bile duct is critical for diagnosing and managing these conditions effectively.
Causes and Risk Factors of Cholecystitis
Cholecystitis primarily results from gallstone obstruction in the cystic duct leading to inflammation of the gallbladder wall, with risk factors including obesity, female gender, rapid weight loss, and age over 40. Bacterial infection may contribute, but the primary cause is often gallstone-related bile stasis. Unlike choledocholithiasis, which involves stones in the common bile duct causing bile duct obstruction and jaundice, cholecystitis is confined to the gallbladder and characterized by localized pain and inflammation.
Causes and Risk Factors of Choledocholithiasis
Choledocholithiasis is primarily caused by gallstones that migrate from the gallbladder into the common bile duct, often developing after gallbladder disease or cholelithiasis. Risk factors include advanced age, obesity, female gender, pregnancy, rapid weight loss, and certain genetic predispositions like hemolytic anemia or bile duct strictures. These factors contribute to bile stasis and increased cholesterol crystallization, fostering stone formation that can lead to bile duct obstruction and subsequent complications.
Key Differences in Pathophysiology
Cholecystitis involves inflammation of the gallbladder wall, primarily caused by cystic duct obstruction from gallstones, leading to bile stasis and gallbladder ischemia. Choledocholithiasis is characterized by the presence of gallstones in the common bile duct, causing bile duct obstruction and potential cholangitis or pancreatitis due to impaired bile flow. The pathophysiology of cholecystitis centers on localized gallbladder inflammation, whereas choledocholithiasis primarily disrupts bile drainage in the biliary tree.
Clinical Presentation: Signs and Symptoms
Cholecystitis typically presents with right upper quadrant abdominal pain, fever, and leukocytosis, often accompanied by nausea and vomiting. Choledocholithiasis commonly manifests as biliary colic, jaundice, dark urine, and pale stools due to bile duct obstruction. Both conditions may cause elevated liver enzymes, but obstructive jaundice is more prominent in choledocholithiasis.
Diagnostic Approaches and Imaging Techniques
Cholecystitis diagnosis primarily relies on ultrasound imaging to detect gallbladder wall thickening, pericholecystic fluid, and sonographic Murphy's sign, while laboratory tests reveal elevated white blood cells and inflammatory markers. Choledocholithiasis diagnosis utilizes magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) to identify bile duct stones and ductal dilatation, supplemented by elevated liver function tests indicating biliary obstruction. Both conditions require precise imaging modalities; ultrasound is first-line for cholecystitis, whereas MRCP and EUS provide superior visualization of bile duct pathology in choledocholithiasis.
Complications and Associated Conditions
Cholecystitis often leads to complications such as gallbladder empyema, gangrene, and perforation, increasing the risk of sepsis and peritonitis. Choledocholithiasis is primarily associated with biliary obstruction, causing cholangitis, pancreatitis, and secondary biliary cirrhosis if untreated. Both conditions can result in jaundice and elevated liver enzymes, but choledocholithiasis poses a higher risk for severe systemic infections due to bile duct obstruction.
Treatment Options and Management Strategies
Cholecystitis treatment typically involves antibiotics to manage infection and laparoscopic cholecystectomy for gallbladder removal, providing definitive resolution. In contrast, choledocholithiasis requires endoscopic retrograde cholangiopancreatography (ERCP) to extract bile duct stones, followed by possible cholecystectomy to prevent recurrence. Supportive care with intravenous fluids, pain management, and monitoring for complications such as cholangitis or pancreatitis is essential in both conditions to optimize patient outcomes.
Prevention and Patient Education
Cholecystitis prevention emphasizes maintaining a healthy diet low in saturated fats to reduce gallstone formation, a primary risk factor, while regular physical activity helps improve bile flow. Choledocholithiasis prevention focuses on early treatment of gallstones and monitoring symptoms like jaundice or abdominal pain to avoid bile duct obstruction. Patient education should highlight recognizing warning signs, understanding the importance of timely medical intervention, and adhering to lifestyle modifications that support biliary health.
Cholecystitis Infographic
 libterm.com
libterm.com