Hyperphosphatemia occurs when phosphate levels in the blood become abnormally high, often due to kidney dysfunction or excessive dietary intake. Managing this condition requires careful monitoring of phosphate levels and dietary adjustments to prevent complications like bone disorders and cardiovascular disease. Discover more about causes, symptoms, and effective treatments to protect your health in the rest of the article.
Table of Comparison
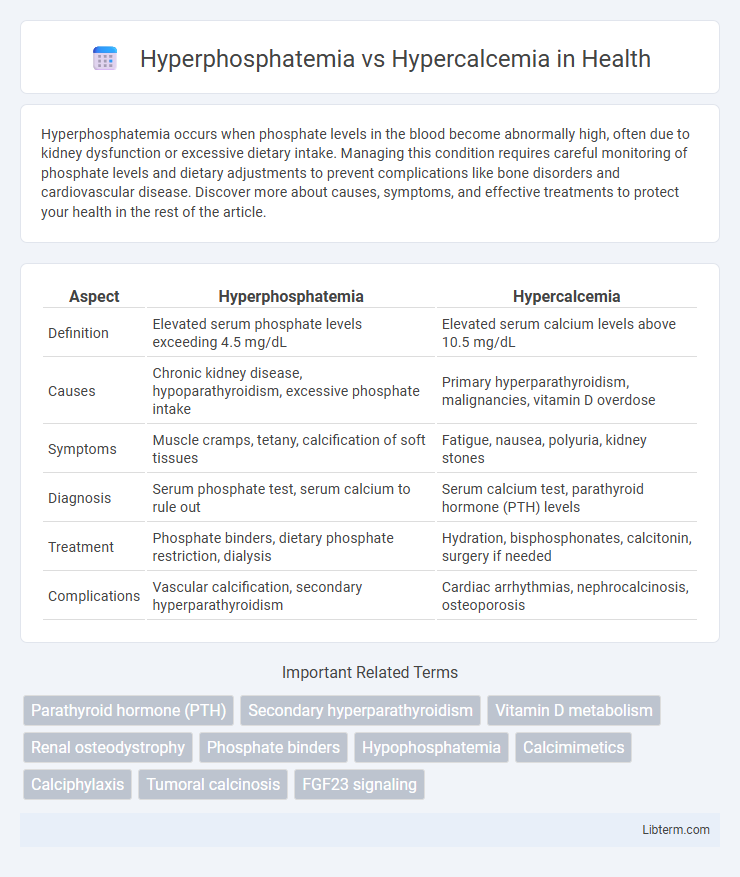
| Aspect | Hyperphosphatemia | Hypercalcemia |
|---|---|---|
| Definition | Elevated serum phosphate levels exceeding 4.5 mg/dL | Elevated serum calcium levels above 10.5 mg/dL |
| Causes | Chronic kidney disease, hypoparathyroidism, excessive phosphate intake | Primary hyperparathyroidism, malignancies, vitamin D overdose |
| Symptoms | Muscle cramps, tetany, calcification of soft tissues | Fatigue, nausea, polyuria, kidney stones |
| Diagnosis | Serum phosphate test, serum calcium to rule out | Serum calcium test, parathyroid hormone (PTH) levels |
| Treatment | Phosphate binders, dietary phosphate restriction, dialysis | Hydration, bisphosphonates, calcitonin, surgery if needed |
| Complications | Vascular calcification, secondary hyperparathyroidism | Cardiac arrhythmias, nephrocalcinosis, osteoporosis |
Introduction to Hyperphosphatemia and Hypercalcemia
Hyperphosphatemia is characterized by elevated serum phosphate levels, often caused by impaired renal excretion, excessive dietary intake, or cellular release due to tissue breakdown. Hypercalcemia involves abnormally high calcium levels in the blood, commonly resulting from hyperparathyroidism, malignancies, or vitamin D intoxication. Both conditions disrupt mineral homeostasis and can lead to significant physiological complications including vascular calcification and neuromuscular disturbances.
Understanding Calcium and Phosphate Homeostasis
Calcium and phosphate homeostasis is regulated primarily by parathyroid hormone (PTH), vitamin D, and fibroblast growth factor 23 (FGF23), balancing their absorption, excretion, and storage. Hyperphosphatemia occurs when phosphate levels rise due to impaired renal excretion or cellular release, disrupting calcium-phosphate balance and potentially causing vascular calcification. Hypercalcemia results from excessive calcium release or absorption, often linked to hyperparathyroidism or malignancies, leading to altered phosphate metabolism and risk of nephrolithiasis and bone resorption.
Causes of Hyperphosphatemia
Hyperphosphatemia primarily results from impaired renal excretion due to chronic kidney disease, excessive dietary phosphate intake, or acute phosphate loads such as tumor lysis syndrome. Other significant causes include hypoparathyroidism, which reduces phosphaturic effects, and vitamin D intoxication, enhancing intestinal phosphate absorption. Understanding these etiologies is crucial for differentiating hyperphosphatemia from hypercalcemia, which typically involves calcium dysregulation rather than phosphate retention.
Causes of Hypercalcemia
Hypercalcemia primarily results from hyperparathyroidism, malignancies such as multiple myeloma or metastatic cancers, and excessive vitamin D intake, leading to elevated calcium levels in the blood. Other causes include certain medications like thiazide diuretics, granulomatous diseases such as sarcoidosis, and immobilization, which increase bone resorption or renal calcium reabsorption. Differentiating from hyperphosphatemia, hypercalcemia disrupts normal calcium-phosphate balance, affecting muscle function and bone health.
Clinical Manifestations: Hyperphosphatemia vs Hypercalcemia
Hyperphosphatemia clinically manifests with symptoms such as muscle cramps, tetany, and pruritus due to its effect on decreasing serum calcium levels and promoting calcium-phosphate deposition in tissues. Hypercalcemia presents with nausea, vomiting, polyuria, neurocognitive disturbances including confusion, and cardiac arrhythmias driven by elevated serum calcium disrupting cellular function. Both conditions require careful monitoring of electrolyte levels to prevent complications like vascular calcification in hyperphosphatemia and cardiac toxicity in hypercalcemia.
Diagnostic Approaches and Key Laboratory Findings
Diagnostic approaches for hyperphosphatemia emphasize measuring elevated serum phosphate levels above 4.5 mg/dL, often coupled with decreased calcium concentrations due to phosphate binding. In contrast, hypercalcemia diagnosis relies on detecting serum calcium levels exceeding 10.5 mg/dL, with potential suppression of parathyroid hormone or elevation in malignancy-related markers. Key laboratory findings include altered calcium-phosphate product ratios, parathyroid hormone assays, vitamin D metabolites, and renal function tests to differentiate underlying causes.
Complications Associated with Both Disorders
Hyperphosphatemia and hypercalcemia both contribute to vascular calcification, significantly increasing the risk of cardiovascular disease in patients with chronic kidney disease. Hyperphosphatemia often leads to secondary hyperparathyroidism and renal osteodystrophy, causing bone fragility and fractures. Hypercalcemia is frequently associated with neurological symptoms, renal stones, and impaired kidney function due to calcium deposition in renal tissues.
Treatment Strategies for Hyperphosphatemia
Treatment strategies for hyperphosphatemia primarily involve dietary phosphate restriction and the use of phosphate binders such as sevelamer, calcium acetate, or lanthanum carbonate to reduce intestinal phosphate absorption. Dialysis is often employed in patients with chronic kidney disease to effectively remove excess phosphate from the bloodstream. Unlike hypercalcemia, which may require intravenous fluids, bisphosphonates, or corticosteroids, hyperphosphatemia management targets lowering serum phosphate levels to prevent vascular calcification and secondary hyperparathyroidism.
Treatment Strategies for Hypercalcemia
Treatment strategies for hypercalcemia primarily involve hydration with intravenous saline to restore volume and promote renal calcium excretion, followed by bisphosphonates to inhibit osteoclast-mediated bone resorption. In severe cases, calcitonin may be administered for rapid calcium reduction, while corticosteroids are effective in hypercalcemia caused by vitamin D excess or certain malignancies. Dialysis is reserved for refractory hypercalcemia or patients with renal failure, ensuring careful correction of electrolyte imbalances.
Prevention and Long-Term Management
Prevention of hyperphosphatemia involves dietary phosphate restriction, use of phosphate binders, and regular monitoring of serum phosphate in patients with chronic kidney disease. Long-term management of hypercalcemia requires identifying and treating underlying causes, maintaining hydration, and avoiding calcium and vitamin D excess. Both conditions benefit from routine laboratory monitoring, patient education on diet and medication adherence, and addressing comorbidities to minimize complications such as vascular calcification and bone disorders.
Hyperphosphatemia Infographic
 libterm.com
libterm.com