Hypoxia occurs when tissues are deprived of adequate oxygen supply, leading to cellular stress and impaired function. Understanding its causes, symptoms, and treatment options is crucial for preventing serious health complications. Explore the rest of the article to learn how hypoxia can affect your body and the strategies to manage it effectively.
Table of Comparison
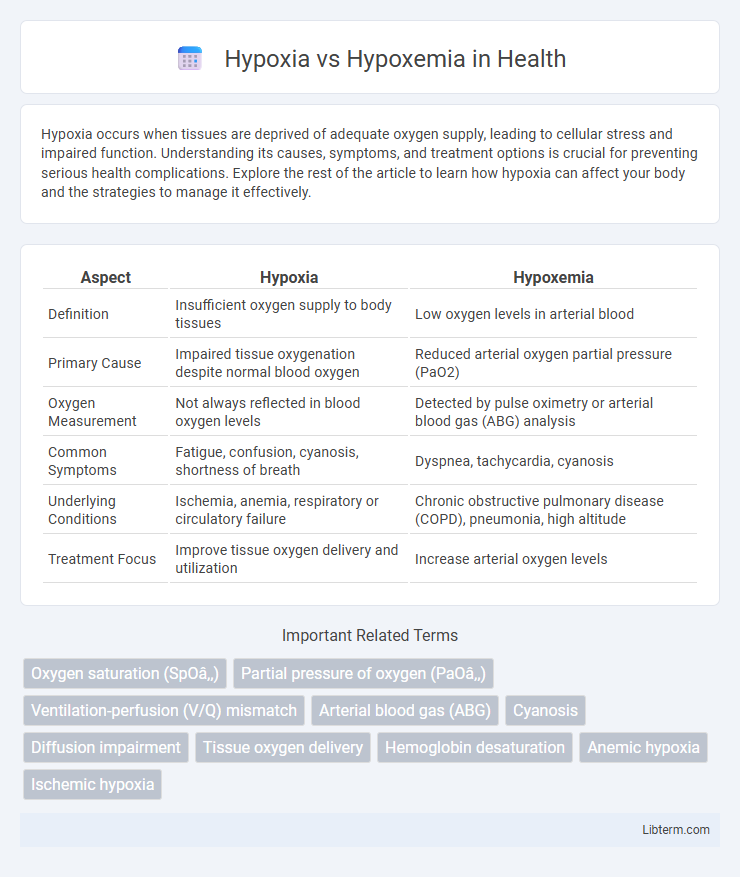
| Aspect | Hypoxia | Hypoxemia |
|---|---|---|
| Definition | Insufficient oxygen supply to body tissues | Low oxygen levels in arterial blood |
| Primary Cause | Impaired tissue oxygenation despite normal blood oxygen | Reduced arterial oxygen partial pressure (PaO2) |
| Oxygen Measurement | Not always reflected in blood oxygen levels | Detected by pulse oximetry or arterial blood gas (ABG) analysis |
| Common Symptoms | Fatigue, confusion, cyanosis, shortness of breath | Dyspnea, tachycardia, cyanosis |
| Underlying Conditions | Ischemia, anemia, respiratory or circulatory failure | Chronic obstructive pulmonary disease (COPD), pneumonia, high altitude |
| Treatment Focus | Improve tissue oxygen delivery and utilization | Increase arterial oxygen levels |
Introduction to Hypoxia and Hypoxemia
Hypoxia refers to a condition where tissues are deprived of adequate oxygen supply despite normal oxygen delivery to the blood. Hypoxemia specifically denotes low levels of oxygen in the arterial blood, measured by a decreased partial pressure of oxygen (PaO2) or oxygen saturation (SpO2). Understanding the distinction between hypoxia and hypoxemia is crucial for diagnosing respiratory or circulatory disorders and managing oxygen therapy effectively.
Definition of Hypoxia
Hypoxia refers to the condition in which there is an inadequate supply of oxygen at the tissue level, impairing cellular function and metabolism. It differs from hypoxemia, which specifically denotes low oxygen levels in arterial blood. Hypoxia can result from various causes, including decreased oxygen delivery, impaired diffusion, or cellular utilization defects.
Definition of Hypoxemia
Hypoxemia is defined as an abnormally low concentration of oxygen in the arterial blood, typically measured by a reduced partial pressure of oxygen (PaO2) below 80 mmHg or a decreased oxygen saturation (SpO2) under 90%. It specifically refers to oxygen deficiency in the bloodstream, which can result from impaired lung function, ventilation-perfusion mismatch, or diffusion defects. Differing from hypoxia, which involves inadequate oxygen supply at the tissue level, hypoxemia is a measurable parameter critical in diagnosing respiratory conditions such as chronic obstructive pulmonary disease (COPD) or acute respiratory distress syndrome (ARDS).
Key Differences Between Hypoxia and Hypoxemia
Hypoxemia refers specifically to low oxygen levels in the blood, typically measured by arterial oxygen tension (PaO2) or oxygen saturation (SpO2), while hypoxia denotes inadequate oxygen supply at the tissue level, impacting cellular metabolism. Key differences include that hypoxemia is a measurable clinical parameter detected via blood gas analysis, whereas hypoxia may occur without hypoxemia if oxygen delivery to tissues is impaired by factors like anemia or circulatory issues. Understanding these distinctions is critical in diagnosing and managing conditions such as chronic obstructive pulmonary disease (COPD), pulmonary embolism, or anemia-related tissue hypoxia.
Causes of Hypoxia
Hypoxia occurs when tissues are deprived of adequate oxygen despite normal or low blood oxygen levels, caused by factors such as impaired oxygen delivery from anemia, carbon monoxide poisoning, or circulatory failure. Hypoxemia specifically refers to low oxygen partial pressure in arterial blood, typically caused by lung diseases like chronic obstructive pulmonary disease (COPD), pneumonia, or ventilation-perfusion mismatch. Understanding the distinction is crucial for targeted treatment, as hypoxia can arise from multiple systemic or cellular dysfunctions beyond just low blood oxygen content.
Causes of Hypoxemia
Hypoxemia, characterized by low arterial oxygen levels, results from causes such as ventilation-perfusion mismatch, diffusion impairment, hypoventilation, and shunt. Common conditions leading to hypoxemia include chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolism, and high-altitude exposure. Understanding these underlying causes is crucial for differentiating hypoxemia from hypoxia and providing targeted treatment.
Signs and Symptoms Comparison
Hypoxia presents with signs such as cyanosis, confusion, rapid breathing, and tachycardia, reflecting inadequate oxygen delivery to tissues despite normal blood oxygen levels. Hypoxemia is characterized by low arterial oxygen saturation detected via pulse oximetry or arterial blood gas analysis, often causing shortness of breath, headache, and altered mental status. Clinical differentiation involves assessing oxygen saturation levels alongside organ dysfunction signs to identify whether reduced oxygen intake or impaired oxygen transport causes the symptoms.
Diagnostic Approaches
Hypoxia diagnosis relies on tissue oxygenation assessment through methods like pulse oximetry and arterial blood gas (ABG) analysis measuring partial pressure of oxygen (PaO2) and oxygen saturation (SaO2). Hypoxemia diagnosis specifically involves measuring PaO2 via ABG and pulse oximetry to detect reduced oxygen content in arterial blood. Imaging studies and clinical examination complement diagnostic evaluation by identifying underlying causes contributing to oxygen deprivation at systemic or cellular levels.
Treatment Strategies for Hypoxia and Hypoxemia
Treatment strategies for hypoxia involve ensuring adequate oxygen delivery to tissues by optimizing ventilation, administering supplemental oxygen, and addressing underlying causes such as anemia or circulatory issues. In managing hypoxemia, treatment focuses on increasing arterial oxygen content through oxygen therapy, mechanical ventilation, and correcting respiratory or cardiac disorders that impair oxygen exchange. Both conditions require prompt evaluation of blood gas levels and targeted interventions to restore sufficient tissue oxygenation and prevent organ damage.
Prevention and Prognosis
Prevention of hypoxia and hypoxemia primarily involves maintaining adequate oxygen delivery through strategies such as avoiding high altitudes without proper acclimatization, controlling chronic respiratory conditions like COPD and asthma, and ensuring timely treatment of cardiac or pulmonary disorders. Prognosis varies depending on the underlying cause and duration; early recognition and intervention often result in favorable outcomes, while prolonged hypoxia can lead to organ damage, neurological deficits, or death. Continuous monitoring of oxygen saturation with pulse oximetry and arterial blood gas analysis is critical for managing these conditions and improving patient prognosis.
Hypoxia Infographic
 libterm.com
libterm.com