Dinoprostone is a prostaglandin used primarily to induce labor by promoting cervical ripening and uterine contractions. This medication plays a crucial role in obstetrics, especially when natural labor needs to be triggered for medical reasons. Explore the detailed uses, benefits, and precautions associated with dinoprostone in the rest of this article.
Table of Comparison
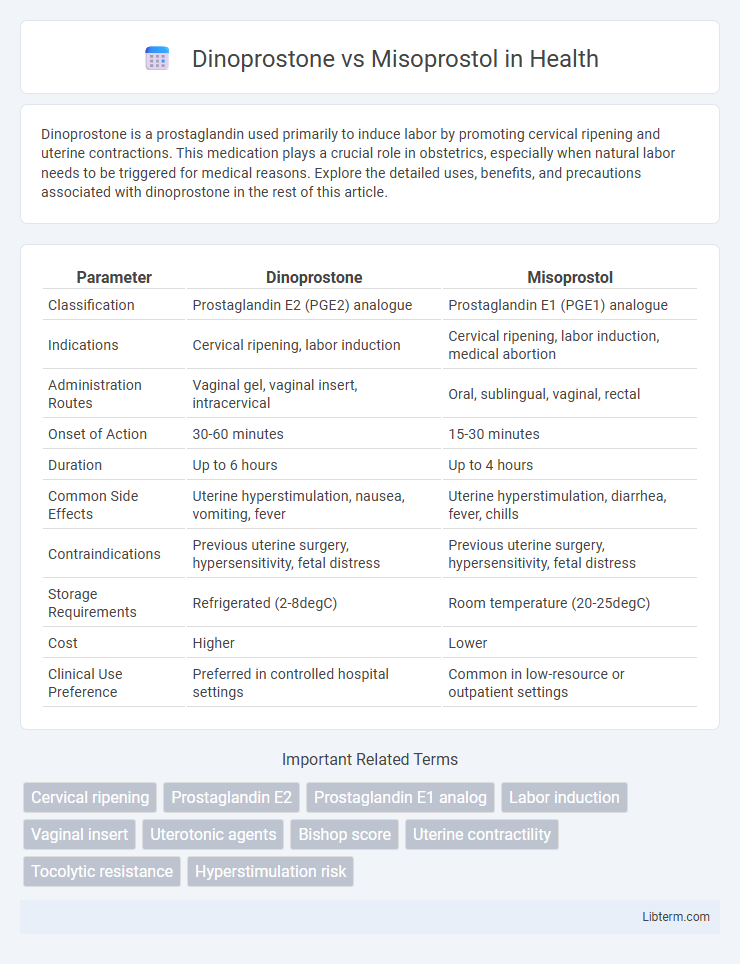
| Parameter | Dinoprostone | Misoprostol |
|---|---|---|
| Classification | Prostaglandin E2 (PGE2) analogue | Prostaglandin E1 (PGE1) analogue |
| Indications | Cervical ripening, labor induction | Cervical ripening, labor induction, medical abortion |
| Administration Routes | Vaginal gel, vaginal insert, intracervical | Oral, sublingual, vaginal, rectal |
| Onset of Action | 30-60 minutes | 15-30 minutes |
| Duration | Up to 6 hours | Up to 4 hours |
| Common Side Effects | Uterine hyperstimulation, nausea, vomiting, fever | Uterine hyperstimulation, diarrhea, fever, chills |
| Contraindications | Previous uterine surgery, hypersensitivity, fetal distress | Previous uterine surgery, hypersensitivity, fetal distress |
| Storage Requirements | Refrigerated (2-8degC) | Room temperature (20-25degC) |
| Cost | Higher | Lower |
| Clinical Use Preference | Preferred in controlled hospital settings | Common in low-resource or outpatient settings |
Introduction to Dinoprostone and Misoprostol
Dinoprostone and Misoprostol are commonly used prostaglandins in obstetrics for cervical ripening and labor induction. Dinoprostone, a natural prostaglandin E2 (PGE2), acts directly on the cervix and myometrium to facilitate dilation and contractions. Misoprostol, a synthetic prostaglandin E1 (PGE1) analog, also induces uterine contractions and is favored for its stability, cost-effectiveness, and broad clinical applications in obstetric management.
Mechanisms of Action
Dinoprostone, a synthetic prostaglandin E2, facilitates cervical ripening and uterine contractions by binding to specific prostaglandin receptors on the uterine smooth muscle, increasing intracellular calcium levels and promoting muscle contraction. Misoprostol, a synthetic prostaglandin E1 analog, exerts its effect by stimulating prostaglandin E receptors, enhancing myometrial contractility and causing cervical softening and dilation through increased production of cyclic AMP and subsequent smooth muscle contraction. Both agents leverage prostaglandin receptor pathways but differ structurally, leading to variations in receptor affinity and clinical usage for labor induction and medical abortion.
Indications and Clinical Uses
Dinoprostone and Misoprostol are both prostaglandins used primarily for cervical ripening and labor induction in obstetrics. Dinoprostone is commonly indicated for inducing labor at term and managing missed miscarriage, whereas Misoprostol is frequently utilized for labor induction, cervical softening, and medical management of first-trimester miscarriage and postpartum hemorrhage. Clinical use of Misoprostol extends to off-label applications due to its stability and lower cost, while Dinoprostone is favored for controlled dosing through vaginal insert or gel formulations.
Efficacy Comparison
Dinoprostone and Misoprostol both effectively induce labor, but Misoprostol demonstrates a higher success rate in cervical ripening and achieving vaginal delivery within 24 hours according to multiple clinical studies. Dinoprostone is associated with a lower risk of uterine hyperstimulation, making it a safer option in patients with uterine scarring or increased risk of complications. Efficacy differences depend on dosage, administration route, and patient-specific factors, with Misoprostol offering greater potency but requiring careful monitoring.
Safety Profiles and Side Effects
Dinoprostone and Misoprostol are both prostaglandins used for cervical ripening and labor induction, but they differ in safety profiles and side effects. Dinoprostone generally has a lower risk of uterine hyperstimulation and fewer gastrointestinal side effects compared to Misoprostol, which is associated with higher incidence of tachysystole and potential fetal distress. Careful dosing and monitoring are crucial with Misoprostol due to its potent uterotonic effects and greater variability in patient response.
Administration Routes and Dosages
Dinoprostone is primarily administered vaginally or intracervically with typical dosages of 10 mg gel or a 3 mg vaginal insert for cervical ripening. Misoprostol is administered orally, buccally, sublingually, or vaginally, with dosages ranging from 25 to 50 mcg every 3 to 6 hours for labor induction. Both drugs require careful dosing adjustments based on patient response and clinical guidelines to minimize adverse effects.
Contraindications and Precautions
Dinoprostone is contraindicated in patients with hypersensitivity to prostaglandins, uterine hypertonus, or unexplained vaginal bleeding, and should be used cautiously in those with previous cesarean section or major uterine surgery due to risks of uterine rupture. Misoprostol is contraindicated in individuals with known allergy to prostaglandins and should be avoided in patients with a history of asthma, cardiovascular disease, or previous uterine surgery due to increased risk of adverse events. Both drugs require careful monitoring during administration in pregnancy to prevent complications such as hyperstimulation and fetal distress.
Maternal and Neonatal Outcomes
Dinoprostone and misoprostol are prostaglandins commonly used for labor induction, with dinoprostone associated with lower rates of uterine hyperstimulation compared to misoprostol, which can lead to adverse neonatal outcomes such as fetal distress. Studies show dinoprostone results in fewer cesarean deliveries and less neonatal intensive care unit (NICU) admissions, indicating improved maternal and neonatal safety profiles. Misoprostol, while effective for cervical ripening, carries a higher risk of tachysystole and subsequent complications, emphasizing the importance of dose and administration route in clinical decision-making.
Cost and Accessibility
Misoprostol is generally more affordable and widely accessible compared to Dinoprostone, making it a preferred choice in low-resource settings for labor induction and medical abortion. Dinoprostone, available mainly under brand names like Cervidil and Prepidil, tends to be more expensive and may require refrigeration, limiting its availability in some regions. The cost-effectiveness and room temperature stability of Misoprostol enhance its usage in diverse healthcare environments worldwide.
Current Guidelines and Recommendations
Current guidelines recommend dinoprostone as the preferred prostaglandin for cervical ripening and labor induction in pregnant women due to its established safety profile and efficacy. Misoprostol is often reserved for settings where dinoprostone is unavailable or contraindicated, with specific dosing regimens to minimize risks of uterine hyperstimulation and fetal distress. Professional organizations, including the American College of Obstetricians and Gynecologists (ACOG), emphasize individualized use based on patient factors, gestational age, and clinical setting to optimize maternal and neonatal outcomes.
Dinoprostone Infographic
 libterm.com
libterm.com