Peptic ulcer disease causes painful sores in the lining of the stomach or duodenum due to excess stomach acid and Helicobacter pylori infection. Effective management includes acid suppression therapy and lifestyle changes that prevent ulcer recurrence and complications. Discover more about symptoms, treatment options, and prevention strategies in the full article.
Table of Comparison
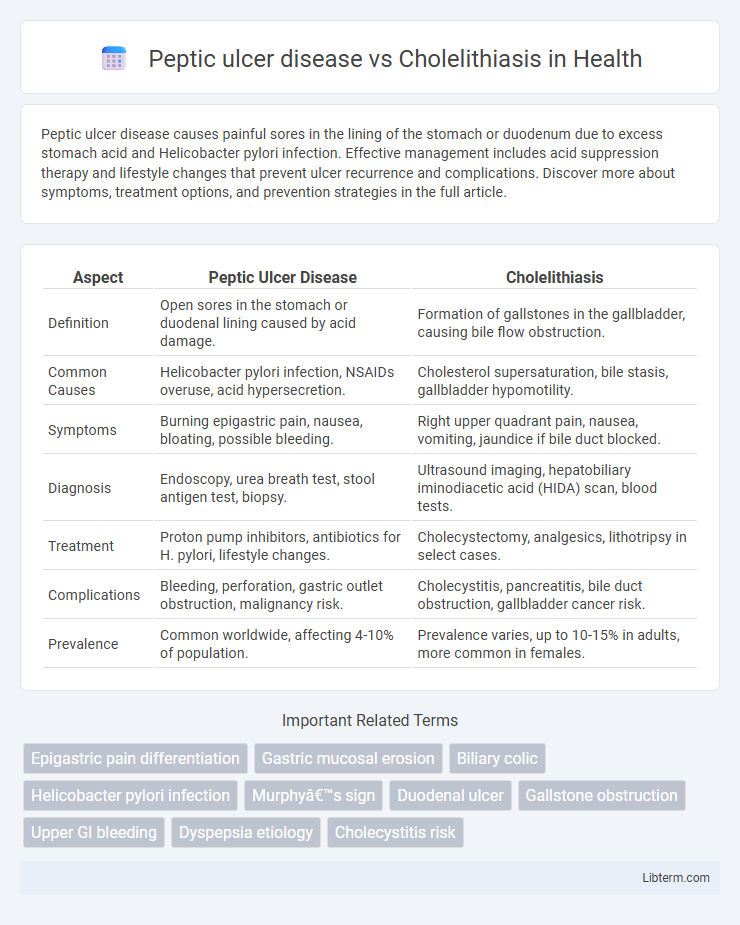
| Aspect | Peptic Ulcer Disease | Cholelithiasis |
|---|---|---|
| Definition | Open sores in the stomach or duodenal lining caused by acid damage. | Formation of gallstones in the gallbladder, causing bile flow obstruction. |
| Common Causes | Helicobacter pylori infection, NSAIDs overuse, acid hypersecretion. | Cholesterol supersaturation, bile stasis, gallbladder hypomotility. |
| Symptoms | Burning epigastric pain, nausea, bloating, possible bleeding. | Right upper quadrant pain, nausea, vomiting, jaundice if bile duct blocked. |
| Diagnosis | Endoscopy, urea breath test, stool antigen test, biopsy. | Ultrasound imaging, hepatobiliary iminodiacetic acid (HIDA) scan, blood tests. |
| Treatment | Proton pump inhibitors, antibiotics for H. pylori, lifestyle changes. | Cholecystectomy, analgesics, lithotripsy in select cases. |
| Complications | Bleeding, perforation, gastric outlet obstruction, malignancy risk. | Cholecystitis, pancreatitis, bile duct obstruction, gallbladder cancer risk. |
| Prevalence | Common worldwide, affecting 4-10% of population. | Prevalence varies, up to 10-15% in adults, more common in females. |
Introduction to Peptic Ulcer Disease and Cholelithiasis
Peptic ulcer disease (PUD) is characterized by mucosal erosions in the stomach or duodenum due to the corrosive effects of gastric acid and pepsin, commonly linked to Helicobacter pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use. Cholelithiasis involves the formation of gallstones within the gallbladder, primarily composed of cholesterol, bilirubin, and calcium salts, often arising from bile supersaturation or gallbladder hypomotility. Both conditions present with abdominal pain but differ in etiology, clinical manifestation, and diagnostic approaches such as endoscopy for PUD and ultrasound imaging for cholelithiasis.
Definition and Overview of Peptic Ulcer Disease
Peptic ulcer disease (PUD) refers to open sores that develop on the inner lining of the stomach, upper small intestine, or esophagus, primarily caused by Helicobacter pylori infection or long-term NSAID use. Cholelithiasis involves the formation of gallstones within the gallbladder, leading to biliary colic or cholecystitis when obstruction occurs. PUD is characterized by epigastric pain, ulceration visible through endoscopy, and complications such as bleeding or perforation, differentiating it from the gallstone-related symptoms in cholelithiasis.
Definition and Overview of Cholelithiasis
Cholelithiasis, commonly known as gallstone disease, involves the formation of solid particles within the gallbladder due to imbalances in bile components such as cholesterol and bile salts. Unlike peptic ulcer disease, which affects the stomach or duodenal lining causing mucosal erosion, cholelithiasis primarily impacts the biliary system leading to symptoms like biliary colic, jaundice, and potential gallbladder inflammation. Accurate diagnosis of cholelithiasis typically relies on abdominal ultrasonography, identifying gallstones and associated complications.
Etiology: Causes and Risk Factors
Peptic ulcer disease primarily arises from Helicobacter pylori infection and chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), with risk factors including smoking, excessive alcohol consumption, and stress. Cholelithiasis is caused by the formation of gallstones due to cholesterol supersaturation, bile stasis, or hemolytic disorders, with risk factors such as obesity, female gender, age over 40, and rapid weight loss. Both conditions involve distinct pathogenetic mechanisms related to gastrointestinal system dysfunction.
Pathophysiology: How Each Disease Develops
Peptic ulcer disease (PUD) develops due to the imbalance between aggressive factors like gastric acid and pepsin and protective mechanisms such as mucus and bicarbonate secretion, often triggered by Helicobacter pylori infection or nonsteroidal anti-inflammatory drug (NSAID) use. Cholelithiasis arises from the supersaturation of bile with cholesterol, bile salts, and phospholipids, leading to the formation of gallstones through nucleation and stone growth within the gallbladder. While PUD primarily involves mucosal injury and inflammation in the gastrointestinal lining, cholelithiasis is characterized by altered bile composition and gallbladder motility dysfunction.
Clinical Presentation: Symptoms and Signs
Peptic ulcer disease typically manifests with epigastric pain described as burning or gnawing, often occurring between meals or at night, accompanied by bloating, nausea, and occasional hematemesis or melena. In contrast, cholelithiasis presents predominantly with episodic right upper quadrant or epigastric pain, particularly after fatty meals, sometimes radiating to the right scapula, alongside nausea and vomiting without significant gastrointestinal bleeding. Physical examination may reveal epigastric tenderness in peptic ulcer disease, whereas Murphy's sign or right upper quadrant tenderness is more common in cholelithiasis.
Diagnostic Approaches and Key Differences
Peptic ulcer disease diagnosis relies heavily on endoscopy to visualize mucosal lesions, with Helicobacter pylori testing essential for identifying bacterial involvement. Cholelithiasis diagnosis primarily utilizes abdominal ultrasound to detect gallstones and assess biliary tract obstruction. Key differences include peptic ulcer disease affecting the gastric or duodenal lining and cholelithiasis involving gallstone formation within the gallbladder, with distinct symptom patterns and imaging modalities guiding diagnosis.
Treatment Strategies for Peptic Ulcer Disease
Treatment strategies for peptic ulcer disease primarily involve eradication of Helicobacter pylori infection using a combination of proton pump inhibitors (PPIs) and antibiotics such as clarithromycin, amoxicillin, or metronidazole. In cases of non-H. pylori ulcers, PPIs alone or H2 receptor antagonists are used to reduce gastric acid secretion and promote mucosal healing. Unlike cholelithiasis, which often requires surgical intervention like cholecystectomy, peptic ulcer disease management emphasizes medication adherence, lifestyle modifications, and monitoring for complications such as bleeding or perforation.
Management Options for Cholelithiasis
Management options for cholelithiasis primarily include conservative measures, pharmacological therapy, and surgical intervention. Asymptomatic gallstones often require no immediate treatment, while symptomatic cases benefit from cholecystectomy, either laparoscopic or open, which remains the definitive therapy. Oral bile acid therapy with ursodeoxycholic acid can be considered for patients who are poor surgical candidates or prefer non-invasive options, although its effectiveness is limited and suitable mainly for cholesterol stones.
Prognosis, Complications, and Prevention
Peptic ulcer disease (PUD) prognosis largely depends on timely treatment with proton pump inhibitors and eradication of Helicobacter pylori, reducing risks of complications like bleeding, perforation, and gastric outlet obstruction. Cholelithiasis prognosis varies with gallstone characteristics; asymptomatic cases may remain stable, but complications include cholecystitis, pancreatitis, and biliary obstruction, often requiring cholecystectomy. Preventive measures for PUD emphasize avoiding NSAIDs and managing H. pylori infection, whereas cholelithiasis prevention focuses on maintaining a healthy weight, balanced diet, and managing lipid levels.
Peptic ulcer disease Infographic
 libterm.com
libterm.com