Metabolic syndrome is a cluster of conditions including high blood pressure, elevated blood sugar, excess body fat around the waist, and abnormal cholesterol levels that increase the risk of heart disease, stroke, and type 2 diabetes. Managing your lifestyle through proper diet, regular exercise, and medical guidance is essential to control and prevent these interconnected health issues. Explore the rest of this article to understand how metabolic syndrome affects your body and the steps you can take to reduce your risks.
Table of Comparison
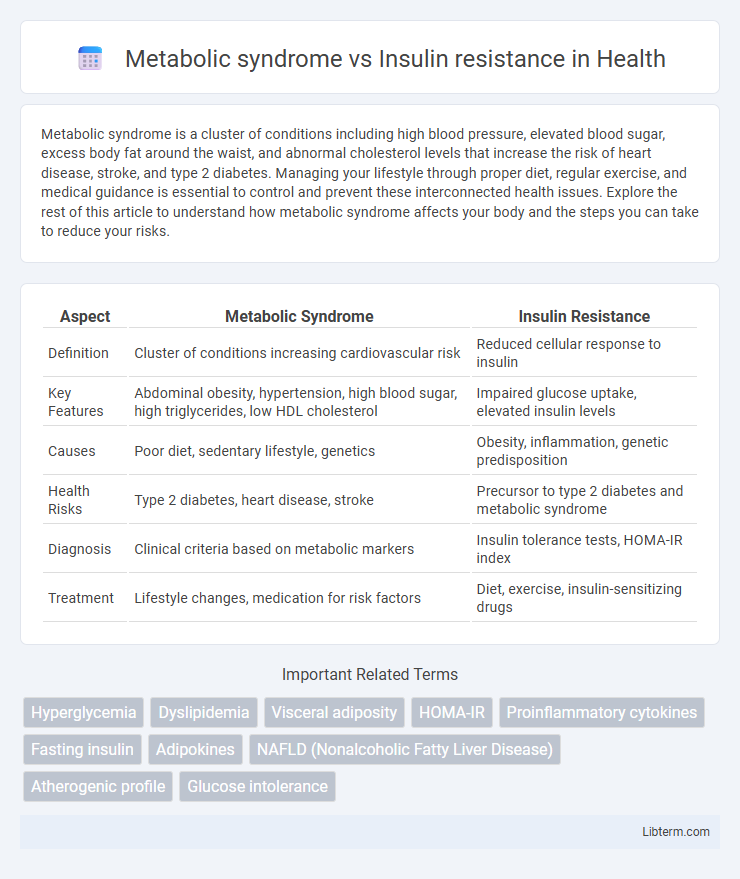
| Aspect | Metabolic Syndrome | Insulin Resistance |
|---|---|---|
| Definition | Cluster of conditions increasing cardiovascular risk | Reduced cellular response to insulin |
| Key Features | Abdominal obesity, hypertension, high blood sugar, high triglycerides, low HDL cholesterol | Impaired glucose uptake, elevated insulin levels |
| Causes | Poor diet, sedentary lifestyle, genetics | Obesity, inflammation, genetic predisposition |
| Health Risks | Type 2 diabetes, heart disease, stroke | Precursor to type 2 diabetes and metabolic syndrome |
| Diagnosis | Clinical criteria based on metabolic markers | Insulin tolerance tests, HOMA-IR index |
| Treatment | Lifestyle changes, medication for risk factors | Diet, exercise, insulin-sensitizing drugs |
Introduction to Metabolic Syndrome and Insulin Resistance
Metabolic syndrome is a cluster of conditions including high blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol levels, which collectively increase the risk of cardiovascular disease and type 2 diabetes. Insulin resistance, a key component of metabolic syndrome, occurs when cells in muscles, fat, and liver do not respond effectively to insulin, leading to elevated blood glucose levels. Understanding the relationship between metabolic syndrome and insulin resistance is critical for early diagnosis and targeted treatment strategies to prevent severe metabolic complications.
Defining Metabolic Syndrome: Criteria and Components
Metabolic syndrome is defined by a cluster of conditions including central obesity, elevated fasting glucose, hypertension, high triglycerides, and low HDL cholesterol that together increase the risk of cardiovascular disease and type 2 diabetes. Insulin resistance is a key underlying mechanism driving metabolic syndrome but represents a single pathological state characterized by reduced cellular response to insulin. The National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria specify that the diagnosis requires at least three of these metabolic abnormalities to qualify as metabolic syndrome.
Understanding Insulin Resistance: Mechanisms and Impact
Insulin resistance occurs when cells in muscles, fat, and liver become less responsive to insulin, causing elevated blood glucose levels and increased insulin production by the pancreas. This impaired insulin signaling disrupts glucose uptake and metabolism, contributing directly to the development of metabolic syndrome--a cluster of conditions including abdominal obesity, hypertension, dyslipidemia, and impaired glucose tolerance. Understanding the molecular mechanisms of insulin resistance, such as inflammation, oxidative stress, and lipid accumulation, is crucial for targeting metabolic syndrome and reducing the risk of type 2 diabetes and cardiovascular disease.
Key Differences Between Metabolic Syndrome and Insulin Resistance
Metabolic syndrome is a cluster of conditions including high blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol levels, whereas insulin resistance specifically refers to the body's reduced response to insulin, leading to impaired glucose uptake. Key differences include that metabolic syndrome encompasses multiple metabolic abnormalities increasing cardiovascular risk, while insulin resistance primarily involves the dysfunction of insulin signaling affecting glucose metabolism. Understanding these distinctions is crucial for targeted interventions in preventing type 2 diabetes and cardiovascular disease.
Shared Risk Factors and Causes
Metabolic syndrome and insulin resistance share key risk factors such as obesity, sedentary lifestyle, and poor dietary habits high in refined sugars and saturated fats. Both conditions are strongly associated with genetic predisposition, chronic inflammation, and hormonal imbalances affecting glucose metabolism. Insulin resistance often acts as a central mechanism driving the development of metabolic syndrome components including hypertension, dyslipidemia, and abdominal obesity.
Clinical Symptoms and Warning Signs
Metabolic syndrome is characterized by a cluster of clinical symptoms including central obesity, elevated blood pressure, high fasting glucose levels, and abnormal lipid profiles such as increased triglycerides and decreased HDL cholesterol. Insulin resistance primarily manifests through signs of impaired glucose metabolism, including acanthosis nigricans, elevated fasting insulin, and postprandial hyperglycemia, often progressing silently before overt symptoms appear. Early warning signs of metabolic syndrome involve persistent hypertension and dyslipidemia, while insulin resistance is typically identified through laboratory markers indicating reduced insulin sensitivity and hyperinsulinemia.
Diagnosis: Tests and Guidelines
Metabolic syndrome diagnosis relies on criteria established by organizations like the National Cholesterol Education Program (NCEP) ATP III, which requires identifying three or more risk factors such as elevated waist circumference, blood pressure, fasting glucose, triglycerides, and low HDL cholesterol. Insulin resistance is primarily assessed using tests like the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) and the hyperinsulinemic-euglycemic clamp, considered the gold standard. Clinical guidelines emphasize early screening of at-risk patients through fasting plasma glucose, HbA1c, and lipid profile tests to detect metabolic syndrome and insulin resistance for timely intervention.
Health Risks and Complications
Metabolic syndrome, characterized by a cluster of conditions including hypertension, abdominal obesity, dyslipidemia, and hyperglycemia, significantly increases the risk of cardiovascular diseases, type 2 diabetes, and stroke. Insulin resistance, a core underlying mechanism of metabolic syndrome, impairs glucose uptake, leading to elevated blood sugar levels and progression toward type 2 diabetes and nonalcoholic fatty liver disease. Both conditions contribute to chronic inflammation and endothelial dysfunction, amplifying the likelihood of atherosclerosis and related cardiovascular complications.
Prevention and Treatment Strategies
Prevention and treatment strategies for metabolic syndrome emphasize lifestyle modifications such as a balanced diet rich in whole grains, fruits, and vegetables combined with regular physical activity to improve insulin sensitivity and reduce cardiovascular risk factors. Insulin resistance management includes targeted interventions like weight loss through caloric restriction, increased muscle activity to enhance glucose uptake, and pharmacological agents such as metformin to improve insulin action. Both conditions benefit from routine monitoring of blood glucose, lipid profiles, and blood pressure to tailor personalized therapeutic approaches that prevent progression to type 2 diabetes and cardiovascular disease.
Conclusion: Managing and Reducing the Risks
Effective management of metabolic syndrome requires targeting multiple risk factors, including obesity, hypertension, dyslipidemia, and high blood glucose levels, to prevent cardiovascular disease and type 2 diabetes. Insulin resistance, a core feature of metabolic syndrome, can be improved through lifestyle interventions such as regular physical activity and a balanced diet rich in fiber and low in refined sugars. Pharmacological therapies may be necessary to control individual components, reducing long-term health risks associated with both conditions.
Metabolic syndrome Infographic
 libterm.com
libterm.com