Rheumatoid arthritis is a chronic inflammatory disorder that primarily affects the joints, causing pain, swelling, and potential loss of function. Early diagnosis and tailored treatment are essential to manage symptoms and prevent joint damage effectively. Discover more about managing rheumatoid arthritis and improving your quality of life in the rest of this article.
Table of Comparison
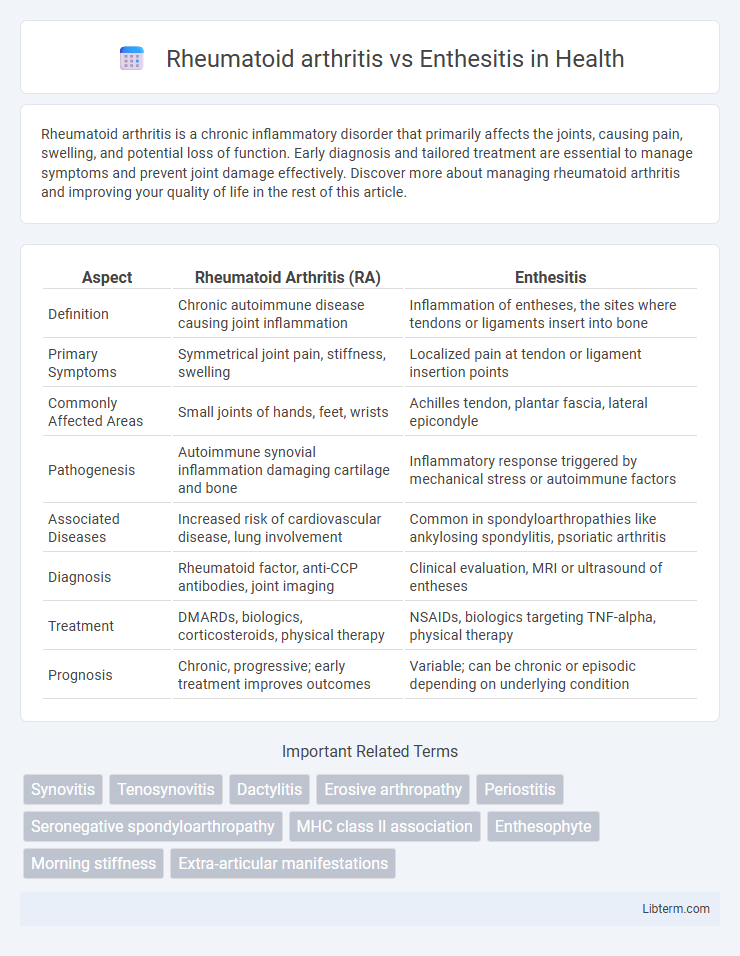
| Aspect | Rheumatoid Arthritis (RA) | Enthesitis |
|---|---|---|
| Definition | Chronic autoimmune disease causing joint inflammation | Inflammation of entheses, the sites where tendons or ligaments insert into bone |
| Primary Symptoms | Symmetrical joint pain, stiffness, swelling | Localized pain at tendon or ligament insertion points |
| Commonly Affected Areas | Small joints of hands, feet, wrists | Achilles tendon, plantar fascia, lateral epicondyle |
| Pathogenesis | Autoimmune synovial inflammation damaging cartilage and bone | Inflammatory response triggered by mechanical stress or autoimmune factors |
| Associated Diseases | Increased risk of cardiovascular disease, lung involvement | Common in spondyloarthropathies like ankylosing spondylitis, psoriatic arthritis |
| Diagnosis | Rheumatoid factor, anti-CCP antibodies, joint imaging | Clinical evaluation, MRI or ultrasound of entheses |
| Treatment | DMARDs, biologics, corticosteroids, physical therapy | NSAIDs, biologics targeting TNF-alpha, physical therapy |
| Prognosis | Chronic, progressive; early treatment improves outcomes | Variable; can be chronic or episodic depending on underlying condition |
Overview of Rheumatoid Arthritis and Enthesitis
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation and progressive joint damage, primarily affecting synovial joints such as the hands and feet. Enthesitis refers to inflammation at the entheses, the sites where tendons or ligaments attach to bone, commonly associated with spondyloarthropathies like ankylosing spondylitis. Both conditions involve immune-mediated inflammation but differ in their primary anatomical targets and underlying pathophysiology.
Key Differences in Disease Definition
Rheumatoid arthritis is a chronic autoimmune disease characterized by symmetrical joint inflammation and synovial membrane damage, primarily affecting small joints in the hands and feet. Enthesitis involves inflammation of the entheses, the sites where tendons or ligaments attach to bone, commonly associated with spondyloarthropathies like ankylosing spondylitis. The key difference lies in rheumatoid arthritis targeting synovial joints with systemic autoimmunity, whereas enthesitis specifically targets entheses, reflecting distinct pathogenic mechanisms and clinical manifestations.
Epidemiology and Demographics
Rheumatoid arthritis (RA) affects approximately 0.5-1% of the global population, predominantly targeting middle-aged women with a female-to-male ratio of about 3:1. Enthesitis, often associated with spondyloarthropathies such as ankylosing spondylitis, is more common in younger males, with prevalence varying widely depending on the underlying condition and geographic region. Both conditions demonstrate distinct epidemiological patterns, with RA showing a higher incidence in Western populations and enthesitis more frequently observed in populations with a higher prevalence of HLA-B27 genetic marker.
Underlying Causes and Risk Factors
Rheumatoid arthritis is an autoimmune disorder characterized by chronic inflammation primarily affecting synovial joints, triggered by a combination of genetic susceptibility, such as HLA-DRB1 gene variants, and environmental factors like smoking. Enthesitis, often associated with spondyloarthropathies such as ankylosing spondylitis, involves inflammation at the entheses, the sites where tendons or ligaments attach to bone, with underlying causes linked to genetic markers like HLA-B27 and mechanical stress. Both conditions share risk factors related to genetic predisposition but differ in immunopathogenesis and specific tissue targets, influencing their clinical presentation and management strategies.
Clinical Manifestations and Symptoms
Rheumatoid arthritis commonly presents with symmetrical joint pain, swelling, stiffness, primarily affecting small joints of the hands and feet, often accompanied by morning stiffness lasting over an hour. Enthesitis is characterized by inflammation at tendon or ligament insertions, causing localized pain and tenderness, frequently affecting sites like the Achilles tendon or plantar fascia, and is often associated with spondyloarthropathies. Both conditions may involve systemic symptoms, but entheseal involvement distinguishes enthesitis, while synovial joint inflammation defines rheumatoid arthritis.
Pathophysiology and Immune Response Mechanisms
Rheumatoid arthritis (RA) primarily involves synovial membrane inflammation driven by autoantibodies such as rheumatoid factor and anti-citrullinated protein antibodies, leading to chronic joint damage through T-cell and B-cell mediated immune responses. Enthesitis, common in spondyloarthropathies, is characterized by inflammation at the enthesis where tendons or ligaments attach to bone, with a dominant role of the innate immune system and involvement of IL-23/IL-17 axis promoting enthesial tissue damage. While RA exhibits systemic autoimmunity targeting joint synovia, enthesitis pathology centers on localized innate immune activation and cytokine-driven inflammation at enthesis sites.
Diagnostic Criteria and Imaging Techniques
Rheumatoid arthritis (RA) diagnosis relies on the 2010 ACR/EULAR classification criteria, emphasizing joint involvement, serology (RF and anti-CCP antibodies), and acute-phase reactants, with ultrasound and MRI aiding in detecting synovitis and erosions. Enthesitis, commonly seen in spondyloarthropathies, is diagnosed based on clinical examination using indices like the MASES or SPARCC and confirmed through ultrasound or MRI, which reveal inflammation at tendon or ligament attachment sites. Imaging techniques for both conditions play a crucial role: MRI offers detailed soft tissue and bone marrow edema visualization in RA, while ultrasound effectively detects entheseal thickening, power Doppler signal, and structural changes in enthesitis.
Treatment Approaches and Management Strategies
Rheumatoid arthritis treatment primarily involves disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, biologics targeting TNF inhibitors, and corticosteroids to reduce joint inflammation and prevent damage. Enthesitis management often includes nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, and biologics like IL-17 or TNF inhibitors to alleviate inflammation at tendon and ligament attachment sites. Both conditions benefit from early diagnosis, personalized treatment plans, and ongoing monitoring to optimize joint function and quality of life.
Long-Term Prognosis and Complications
Rheumatoid arthritis (RA) often leads to chronic joint damage, deformities, and increased risk of cardiovascular disease, significantly impacting long-term function and quality of life. Enthesitis, common in spondyloarthropathies, primarily affects tendon and ligament insertion sites causing persistent pain and potential new bone formation or fusion but generally preserves joint architecture better than RA. Early diagnosis and targeted treatment are crucial for both conditions to minimize complications such as joint destruction in RA and ankylosis or spinal rigidity in enthesitis-associated disorders.
Patient Lifestyle and Coping Strategies
Rheumatoid arthritis (RA) patients often benefit from structured physical therapy and balanced exercise routines to maintain joint flexibility and reduce pain, while those with enthesitis focus on targeted stretching and low-impact activities to manage inflammation at tendon attachment sites. Both conditions require tailored dietary plans rich in anti-inflammatory foods like omega-3 fatty acids and antioxidants to support immune system modulation and symptom control. Stress reduction techniques such as mindfulness and adequate rest are crucial coping strategies that improve overall quality of life and reduce disease flares in RA and enthesitis patients.
Rheumatoid arthritis Infographic
 libterm.com
libterm.com