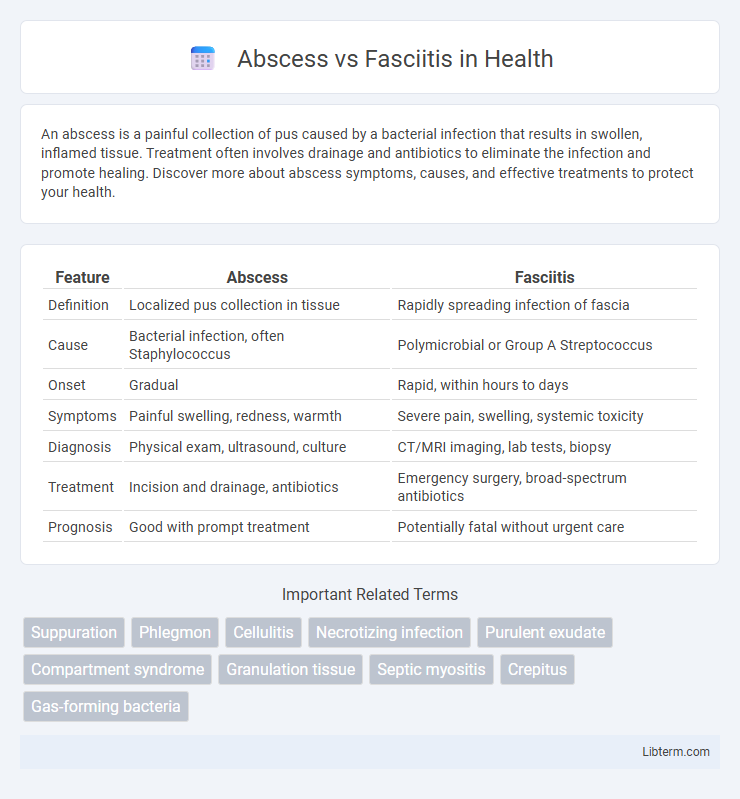
An abscess is a painful collection of pus caused by a bacterial infection that results in swollen, inflamed tissue. Treatment often involves drainage and antibiotics to eliminate the infection and promote healing. Discover more about abscess symptoms, causes, and effective treatments to protect your health.
Table of Comparison
| Feature | Abscess | Fasciitis |
|---|---|---|
| Definition | Localized pus collection in tissue | Rapidly spreading infection of fascia |
| Cause | Bacterial infection, often Staphylococcus | Polymicrobial or Group A Streptococcus |
| Onset | Gradual | Rapid, within hours to days |
| Symptoms | Painful swelling, redness, warmth | Severe pain, swelling, systemic toxicity |
| Diagnosis | Physical exam, ultrasound, culture | CT/MRI imaging, lab tests, biopsy |
| Treatment | Incision and drainage, antibiotics | Emergency surgery, broad-spectrum antibiotics |
| Prognosis | Good with prompt treatment | Potentially fatal without urgent care |
Understanding Abscess and Fasciitis: Definitions
An abscess is a localized collection of pus caused by bacterial infection, resulting in swelling, redness, and pain, often requiring drainage for treatment. Fasciitis refers to the inflammation of the fascia, a connective tissue surrounding muscles, commonly seen in necrotizing fasciitis, a rapidly spreading bacterial infection that destroys tissue. Differentiating between abscess and fasciitis is crucial for timely medical intervention due to their distinct pathophysiology and treatment approaches.
Key Differences Between Abscess and Fasciitis
An abscess is a localized collection of pus caused by bacterial infection, often presenting as a painful, swollen lump, whereas fasciitis is a severe, rapidly spreading inflammation of the fascia, typically caused by aggressive bacterial pathogens like Group A Streptococcus. Abscesses generally require drainage and antibiotics, while necrotizing fasciitis demands urgent surgical debridement alongside intensive antibiotic therapy due to its life-threatening nature. Diagnostic imaging such as ultrasound or MRI can help differentiate an abscess's fluid-filled cavity from the diffuse fascial thickening and gas presence characteristic of fasciitis.
Causes and Risk Factors
Abscesses are typically caused by bacterial infections, such as Staphylococcus aureus, leading to localized pus accumulation due to immune response, while necrotizing fasciitis results from rapidly spreading bacterial infections, often involving Group A Streptococcus, that destroy fascia and soft tissue. Risk factors for abscess formation include poor hygiene, immune suppression, and chronic skin conditions, whereas fasciitis risk factors encompass recent trauma, surgery, diabetes, and compromised immune systems. Both conditions are serious, but necrotizing fasciitis progresses more aggressively, requiring prompt diagnosis and treatment to prevent systemic complications.
Clinical Presentation and Symptoms
Abscess typically presents as a localized, painful, swollen area with fluctuance and erythema, often accompanied by fever and tenderness. Fasciitis, particularly necrotizing fasciitis, manifests with rapidly progressing pain that is disproportionate to physical findings, swelling, erythema, and systemic symptoms such as fever, hypotension, and tachycardia. Early signs of fasciitis include severe pain, edema beyond skin erythema, and skin discoloration, distinguishing it from the more contained and palpable abscess.
Diagnostic Methods for Identification
Diagnosis of abscess primarily involves clinical examination combined with ultrasound imaging to detect fluid collections and confirm pus accumulation. In contrast, necrotizing fasciitis requires prompt recognition using contrast-enhanced MRI or CT scans to identify fascial thickening, gas formation, and soft tissue edema. Laboratory studies including elevated white blood cell count and C-reactive protein levels support differentiation, while definitive diagnosis for fasciitis often depends on surgical exploration and tissue biopsy.
Imaging Techniques: Ultrasound vs. MRI
Ultrasound is effective for initial evaluation of abscesses, providing real-time imaging to detect fluid collections and guide needle aspiration, especially in superficial soft tissue infections. MRI offers superior soft tissue contrast and detailed visualization critical for diagnosing necrotizing fasciitis, revealing fascial thickening, edema, and gas formation, which are often missed on ultrasound. Combining both modalities enhances diagnostic accuracy by leveraging ultrasound's accessibility and MRI's comprehensive assessment of disease extent.
Treatment Approaches for Abscess
Treatment approaches for abscess primarily focus on drainage of the pus to relieve pressure and eliminate infection, typically through incision and drainage (I&D). Antibiotic therapy is used adjunctively, especially in cases of systemic infection or immunocompromised patients, to target causative bacteria like Staphylococcus aureus and Streptococcus species. Proper wound care and follow-up are essential to prevent recurrence and promote healing.
Treatment Strategies for Fasciitis
Fasciitis requires aggressive treatment strategies including high-dose intravenous antibiotics targeting Group A Streptococcus and anaerobic bacteria, combined with urgent surgical debridement to remove necrotic tissue and prevent systemic spread. Hyperbaric oxygen therapy may be utilized to enhance tissue oxygenation and support wound healing in severe cases. Early diagnosis and multidisciplinary management are crucial to improve outcomes and reduce mortality associated with necrotizing fasciitis.
Complications and Prognosis Comparison
Abscesses typically cause localized infection with pus formation that can lead to tissue destruction but usually respond well to drainage and antibiotics, resulting in a favorable prognosis. Fasciitis, particularly necrotizing fasciitis, is a rapidly progressing soft tissue infection involving fascial planes that can cause widespread tissue necrosis, systemic toxicity, and potential multi-organ failure, leading to a high risk of mortality. Complications of fasciitis are more severe and rapid compared to abscesses, with fasciitis often requiring aggressive surgical debridement and intensive care to improve survival chances.
Prevention and Early Detection Tips
Effective prevention of abscesses and fasciitis involves maintaining proper hygiene, promptly treating skin wounds, and avoiding unnecessary invasive procedures. Early detection signs of abscess include localized swelling, redness, and pain, while fasciitis often presents with rapidly spreading severe pain, fever, and skin discoloration. Seeking immediate medical evaluation and intervention at these early symptoms significantly reduces complications and improves treatment outcomes.
Abscess Infographic
 libterm.com
libterm.com