An autoimmune response occurs when the immune system mistakenly attacks the body's own healthy cells, causing inflammation and tissue damage. Understanding the triggers, symptoms, and treatment options is crucial for managing conditions related to autoimmune disorders effectively. Explore the rest of the article to learn how you can recognize and address autoimmune responses for better health.
Table of Comparison
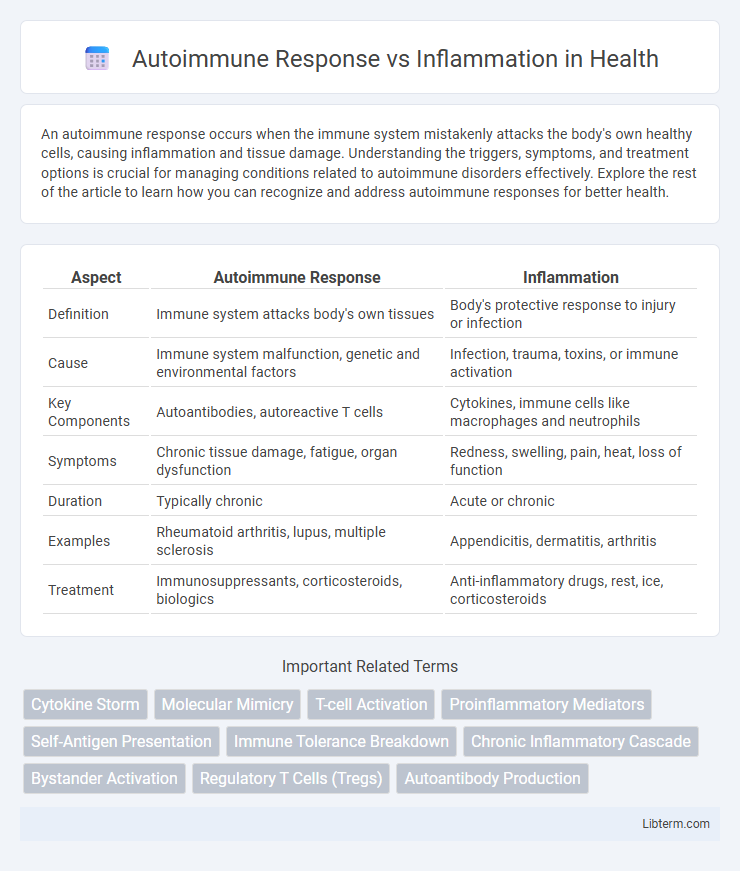
| Aspect | Autoimmune Response | Inflammation |
|---|---|---|
| Definition | Immune system attacks body's own tissues | Body's protective response to injury or infection |
| Cause | Immune system malfunction, genetic and environmental factors | Infection, trauma, toxins, or immune activation |
| Key Components | Autoantibodies, autoreactive T cells | Cytokines, immune cells like macrophages and neutrophils |
| Symptoms | Chronic tissue damage, fatigue, organ dysfunction | Redness, swelling, pain, heat, loss of function |
| Duration | Typically chronic | Acute or chronic |
| Examples | Rheumatoid arthritis, lupus, multiple sclerosis | Appendicitis, dermatitis, arthritis |
| Treatment | Immunosuppressants, corticosteroids, biologics | Anti-inflammatory drugs, rest, ice, corticosteroids |
Understanding Autoimmune Response
Autoimmune response occurs when the immune system mistakenly targets the body's own tissues, leading to chronic inflammation and tissue damage. Key immune components involved include autoreactive T cells, autoantibodies, and cytokines that perpetuate the immune attack. Understanding the mechanisms of immune tolerance breakdown and antigen presentation offers insights into autoimmune diseases like rheumatoid arthritis and multiple sclerosis.
What Is Inflammation?
Inflammation is the body's natural immune response to injury or infection, characterized by redness, swelling, heat, and pain at the affected site. It involves the activation of immune cells, release of signaling molecules like cytokines, and increased blood flow to eliminate harmful stimuli and promote tissue repair. Unlike autoimmune responses, which mistakenly target the body's own tissues, inflammation is a protective mechanism aimed at restoring health and fighting off pathogens.
Key Differences Between Autoimmune Response and Inflammation
An autoimmune response occurs when the immune system mistakenly targets the body's own cells, leading to chronic tissue damage, whereas inflammation is the body's protective reaction to injury or infection primarily involving immune cell activation and release of signaling molecules. Autoimmune responses are characterized by the production of autoantibodies and self-reactive T cells, whereas inflammation is marked by localized redness, swelling, heat, and pain due to increased blood flow and immune cell infiltration. Unlike general inflammation, autoimmune responses are sustained and can cause systemic effects, contributing to chronic diseases such as rheumatoid arthritis and lupus.
Causes of Autoimmune Responses
Autoimmune responses are triggered when the immune system mistakenly identifies the body's own cells as foreign, leading to the production of autoantibodies and autoreactive T-cells. Genetic predispositions, such as specific HLA alleles, combined with environmental factors like infections, toxins, or stress, frequently initiate these responses. Unlike general inflammation driven by injury or infection, autoimmune inflammation results from a breakdown in immune tolerance and persistent immune activation against self-antigens.
Triggers and Types of Inflammation
Autoimmune response occurs when the immune system mistakenly attacks healthy tissues, triggered by genetic predisposition, infections, or environmental factors, leading to chronic inflammation. Inflammation types include acute, characterized by rapid onset and resolution, and chronic, marked by prolonged tissue damage often seen in autoimmune diseases like rheumatoid arthritis and lupus. Common triggers of inflammation involve pathogens, toxins, and persistent immune activation, which differ in autoimmune cases where self-antigens provoke sustained immune reactions.
How Autoimmune Disorders Affect the Body
Autoimmune disorders trigger the immune system to mistakenly attack healthy tissues, causing persistent inflammation that damages organs and disrupts normal bodily functions. Chronic inflammation resulting from this immune dysregulation leads to symptoms such as pain, swelling, and tissue degeneration, which can progressively impair organ systems like joints in rheumatoid arthritis or the nervous system in multiple sclerosis. Effective management targets both the autoimmune response and the resulting inflammatory processes to prevent long-term tissue destruction and maintain physiological balance.
Role of Inflammation in Disease
Inflammation acts as a critical mediator in autoimmune diseases by triggering immune cells to attack healthy tissues, leading to chronic damage and dysfunction. Persistent inflammation results in the release of cytokines and chemokines that amplify immune responses and contribute to disease progression in conditions like rheumatoid arthritis and lupus. Targeting inflammatory pathways with biologic therapies helps to reduce tissue injury and control autoimmune disease symptoms effectively.
Diagnostic Methods: Autoimmune vs Inflammatory Conditions
Diagnostic methods for autoimmune conditions typically involve detecting specific autoantibodies through tests like ANA (antinuclear antibody) or RF (rheumatoid factor), alongside imaging and biopsy to identify tissue damage caused by immune attack. Inflammatory conditions are often diagnosed by measuring markers such as CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate), which indicate acute or chronic inflammation without pinpointing immune system specificity. Advanced techniques like flow cytometry and cytokine profiling enhance differentiation by characterizing immune cell populations and inflammatory mediator profiles unique to autoimmune versus non-autoimmune inflammation.
Treatment Approaches for Autoimmune and Inflammatory Diseases
Treatment approaches for autoimmune diseases primarily involve immunosuppressive medications such as corticosteroids, methotrexate, and biologics targeting specific immune pathways like TNF inhibitors, which help reduce the autoimmune response by modulating overactive immune cells. Inflammatory diseases often require anti-inflammatory drugs including NSAIDs and corticosteroids to alleviate symptoms by decreasing inflammation and pain, along with lifestyle modifications and physical therapy to improve function. Advanced therapies like monoclonal antibodies and small molecule inhibitors are increasingly used in both autoimmune and inflammatory conditions to target precise molecular mechanisms and improve patient outcomes.
Preventing Chronic Autoimmunity and Inflammation
Preventing chronic autoimmunity and inflammation involves regulating immune system activity to avoid persistent tissue damage and immune dysregulation. Therapeutic strategies targeting cytokine signaling pathways, such as TNF-a inhibitors and IL-6 blockers, reduce chronic inflammatory responses and autoantibody production. Lifestyle interventions including balanced nutrition, stress management, and avoiding environmental triggers support immune homeostasis and minimize chronic autoimmune activation.
Autoimmune Response Infographic
 libterm.com
libterm.com