Gastroparesis and functional dyspepsia are digestive disorders that significantly affect stomach motility and cause chronic discomfort such as nausea, bloating, and early satiety. Understanding the differences in their causes, symptoms, and treatment options helps tailor effective management strategies for your digestive health. Explore the full article to learn how to identify, manage, and improve quality of life when facing these conditions.
Table of Comparison
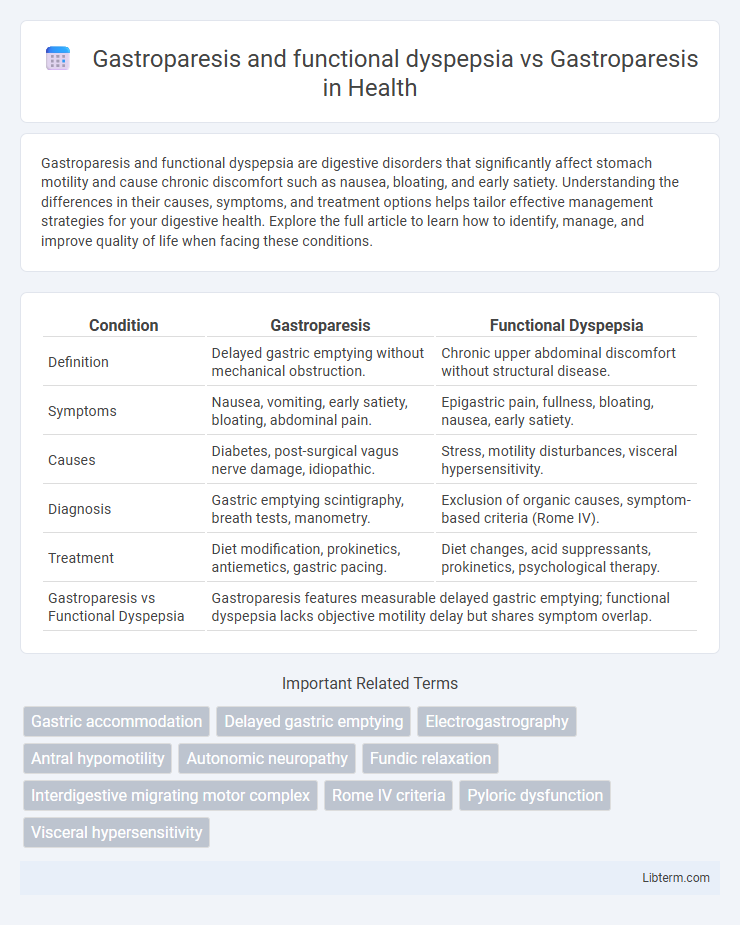
| Condition | Gastroparesis | Functional Dyspepsia |
|---|---|---|
| Definition | Delayed gastric emptying without mechanical obstruction. | Chronic upper abdominal discomfort without structural disease. |
| Symptoms | Nausea, vomiting, early satiety, bloating, abdominal pain. | Epigastric pain, fullness, bloating, nausea, early satiety. |
| Causes | Diabetes, post-surgical vagus nerve damage, idiopathic. | Stress, motility disturbances, visceral hypersensitivity. |
| Diagnosis | Gastric emptying scintigraphy, breath tests, manometry. | Exclusion of organic causes, symptom-based criteria (Rome IV). |
| Treatment | Diet modification, prokinetics, antiemetics, gastric pacing. | Diet changes, acid suppressants, prokinetics, psychological therapy. |
| Gastroparesis vs Functional Dyspepsia | Gastroparesis features measurable delayed gastric emptying; functional dyspepsia lacks objective motility delay but shares symptom overlap. | |
Understanding Gastroparesis: Definition and Causes
Gastroparesis is a disorder characterized by delayed gastric emptying without mechanical obstruction, often caused by nerve damage, diabetes, or viral infections. Functional dyspepsia involves chronic upper abdominal discomfort with normal gastric emptying but impaired gastric accommodation and hypersensitivity. Unlike functional dyspepsia, gastroparesis primarily results from disrupted autonomic nervous system function, leading to symptoms such as nausea, vomiting, and early satiety.
What is Functional Dyspepsia? Key Features and Triggers
Functional dyspepsia is a common gastrointestinal disorder characterized by chronic or recurrent upper abdominal discomfort or pain without an identifiable organic cause, often overlapping with symptoms of gastroparesis. Key features include early satiety, postprandial fullness, bloating, and nausea, which significantly impair quality of life. Triggers for functional dyspepsia typically involve dietary factors, stress, and disturbed gastric motility, distinguishing it from gastroparesis that primarily involves delayed gastric emptying evidenced through diagnostic gastric emptying studies.
Gastroparesis vs. Functional Dyspepsia: Core Differences
Gastroparesis and functional dyspepsia both involve upper gastrointestinal symptoms but differ significantly in pathophysiology and diagnostic criteria. Gastroparesis is characterized by delayed gastric emptying confirmed through gastric emptying scintigraphy, often linked to nerve damage such as vagus nerve dysfunction, whereas functional dyspepsia presents with similar symptoms without delayed gastric emptying or structural abnormalities. Treatment approaches for gastroparesis focus on improving gastric motility using prokinetic agents, while functional dyspepsia management targets symptom relief through dietary modifications and acid suppression therapies.
Overlapping Symptoms: When Gastroparesis and Dyspepsia Collide
Gastroparesis and functional dyspepsia share overlapping symptoms such as delayed gastric emptying, nausea, bloating, and early satiety, complicating differential diagnosis. Both conditions can present with upper abdominal discomfort and fullness, yet gastroparesis is distinguished by objectively measured delayed gastric motility via gastric emptying studies. Accurate identification of symptom overlap between gastroparesis and functional dyspepsia is critical for targeted treatment and improved patient outcomes.
Diagnostic Challenges: Differentiating the Two Conditions
Diagnosing gastroparesis and functional dyspepsia presents significant challenges due to overlapping symptoms such as nausea, early satiety, and postprandial fullness. Gastroparesis is characterized by delayed gastric emptying confirmed through gastric emptying scintigraphy, whereas functional dyspepsia lacks objective abnormalities on diagnostic tests, relying primarily on symptom criteria like the Rome IV guidelines. Differentiating these conditions requires careful evaluation of gastric motility, symptom patterns, and exclusion of mechanical obstruction or systemic diseases.
Role of Gastric Motility in Gastroparesis vs. Functional Dyspepsia
Gastroparesis is characterized by delayed gastric emptying due to impaired gastric motility caused by vagus nerve dysfunction or smooth muscle abnormalities. Functional dyspepsia presents with normal gastric emptying but involves impaired gastric accommodation and hypersensitivity, impacting gastric motility patterns differently than gastroparesis. The role of gastric motility in gastroparesis centers on delayed transit and motility failure, whereas in functional dyspepsia, altered motility relates to impaired gastric relaxation and sensory dysfunction without significant emptying delay.
Impact on Quality of Life: Patient Experiences
Gastroparesis significantly impairs quality of life through chronic nausea, vomiting, and severe gastric motility delays, leading to poor nutritional status and frequent hospitalizations. Functional dyspepsia, while characterized by upper abdominal discomfort and early satiety, usually involves less severe gastric emptying abnormalities but still causes persistent pain and emotional distress. Patients with gastroparesis often report more profound limitations in daily activities and social interactions compared to those with functional dyspepsia, reflecting the greater severity of symptoms and dietary restrictions.
Treatment Approaches: Tailoring Therapy to Each Condition
Treatment approaches for gastroparesis primarily focus on prokinetic agents like metoclopramide or erythromycin to enhance gastric motility, alongside dietary modifications such as small, frequent meals low in fat and fiber. Functional dyspepsia management emphasizes acid suppression with proton pump inhibitors or H2 receptor antagonists and symptomatic relief using prokinetics or neuromodulators like tricyclic antidepressants for visceral hypersensitivity. Tailoring therapy requires accurate diagnosis through gastric emptying studies and symptom assessment to distinguish delayed gastric emptying in gastroparesis from normal gastric emptying with dyspeptic symptoms in functional dyspepsia.
Prognosis and Long-Term Management Strategies
Gastroparesis and functional dyspepsia both involve impaired gastric motility but differ significantly in prognosis and long-term management. Gastroparesis often requires sustained prokinetic therapy, dietary modifications, and sometimes gastric electrical stimulation or feeding tube placement due to its chronic, progressive nature and risk of malnutrition. Functional dyspepsia generally has a more favorable prognosis with symptom-oriented treatments like acid suppression, prokinetics, and lifestyle changes, focusing on symptom relief without the extensive complications seen in gastroparesis.
Emerging Research: Advances in Gastroparesis and Dyspepsia Understanding
Emerging research in gastroparesis and functional dyspepsia reveals distinct pathophysiological mechanisms, highlighting delayed gastric emptying in gastroparesis compared to visceral hypersensitivity in functional dyspepsia. Advances in diagnostic techniques, such as gastric scintigraphy and electrogastrography, enhance differentiation between these disorders. Novel therapeutic targets, including neuromodulators and prokinetic agents, are under investigation to improve symptom management and patient outcomes.
Gastroparesis and functional dyspepsia Infographic
 libterm.com
libterm.com