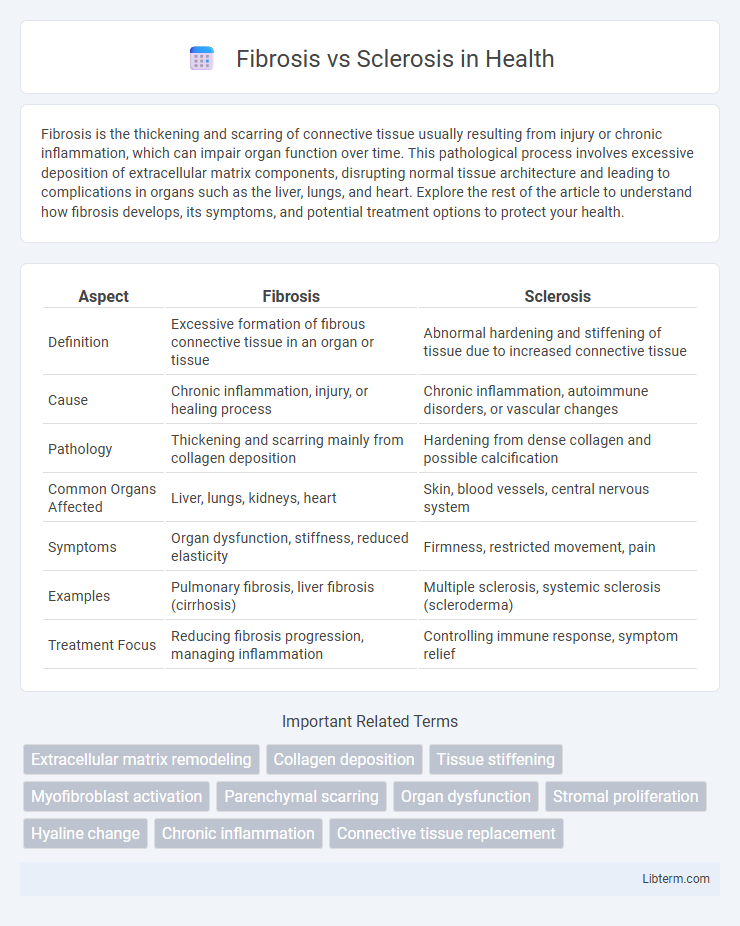
Fibrosis is the thickening and scarring of connective tissue usually resulting from injury or chronic inflammation, which can impair organ function over time. This pathological process involves excessive deposition of extracellular matrix components, disrupting normal tissue architecture and leading to complications in organs such as the liver, lungs, and heart. Explore the rest of the article to understand how fibrosis develops, its symptoms, and potential treatment options to protect your health.
Table of Comparison
| Aspect | Fibrosis | Sclerosis |
|---|---|---|
| Definition | Excessive formation of fibrous connective tissue in an organ or tissue | Abnormal hardening and stiffening of tissue due to increased connective tissue |
| Cause | Chronic inflammation, injury, or healing process | Chronic inflammation, autoimmune disorders, or vascular changes |
| Pathology | Thickening and scarring mainly from collagen deposition | Hardening from dense collagen and possible calcification |
| Common Organs Affected | Liver, lungs, kidneys, heart | Skin, blood vessels, central nervous system |
| Symptoms | Organ dysfunction, stiffness, reduced elasticity | Firmness, restricted movement, pain |
| Examples | Pulmonary fibrosis, liver fibrosis (cirrhosis) | Multiple sclerosis, systemic sclerosis (scleroderma) |
| Treatment Focus | Reducing fibrosis progression, managing inflammation | Controlling immune response, symptom relief |
Understanding Fibrosis and Sclerosis: Key Definitions
Fibrosis is the excessive accumulation of fibrous connective tissue in an organ or tissue as a reparative response to injury or chronic inflammation, often leading to impaired function. Sclerosis refers to the abnormal hardening of body tissues, frequently resulting from the thickening and stiffening of connective tissue, which can restrict normal organ flexibility and function. Understanding these definitions is crucial for diagnosing conditions such as liver cirrhosis (fibrosis) and multiple sclerosis (sclerosis), where tissue changes play a central role in disease progression.
Causes and Risk Factors of Fibrosis and Sclerosis
Fibrosis results from chronic inflammation or tissue injury leading to excessive collagen deposition, commonly caused by factors such as chronic infections, autoimmune diseases, radiation exposure, and environmental toxins. Sclerosis involves abnormal hardening of tissue due to increased fibrous tissue formation, often linked to autoimmune disorders like systemic sclerosis, atherosclerosis, and multiple sclerosis as key risk factors. Both conditions share underlying mechanisms related to immune system dysregulation and persistent tissue damage but differ in tissue localization and specific triggers.
Pathophysiology: How Fibrosis Differs from Sclerosis
Fibrosis involves the excessive accumulation of extracellular matrix components, primarily collagen, due to chronic inflammation or tissue injury, leading to tissue scarring and impaired organ function. Sclerosis primarily denotes the hardening and thickening of tissue caused by increased fibrous tissue or calcification, often resulting from chronic inflammatory or autoimmune processes. Unlike sclerosis, fibrosis is characterized by active fibroblast proliferation and matrix deposition, while sclerosis emphasizes structural rigidity and loss of elasticity in affected tissues.
Common Types of Fibrosis and Sclerosis Disorders
Fibrosis commonly occurs in organs such as the liver (hepatic fibrosis), lungs (pulmonary fibrosis), and kidneys (renal fibrosis), characterized by excessive extracellular matrix deposition leading to tissue scarring and impaired function. Sclerosis disorders include systemic sclerosis (scleroderma), characterized by hardening and tightening of the skin and connective tissues, and multiple sclerosis, an autoimmune disease affecting nerve cell communication through demyelination. Both fibrosis and sclerosis involve pathological tissue remodeling but differ in their primary affected tissues and underlying mechanisms.
Symptoms and Clinical Manifestations
Fibrosis manifests through symptoms such as persistent tissue stiffness, reduced organ functionality, and chronic inflammation, often leading to scarring and impaired physiological processes. Sclerosis primarily presents with symptoms of abnormal hardening and thickening of tissues, resulting in restricted movement, pain, and potential nerve compression depending on the affected site. Clinical manifestations of fibrosis typically involve progressive organ dysfunction, while sclerosis is characterized by firm, often palpable indurations and structural tissue rigidity.
Diagnostic Methods: Identifying Fibrosis and Sclerosis
Diagnostic methods for fibrosis include imaging techniques like ultrasound elastography and magnetic resonance elastography, which assess tissue stiffness indicative of fibrotic changes. Sclerosis diagnosis often relies on clinical examination combined with biopsy to confirm abnormal hardening and increased collagen deposition in tissues. Laboratory tests measuring specific biomarkers and autoantibodies complement imaging and histological analyses to differentiate between fibrosis and sclerosis accurately.
Treatment Approaches: Managing Fibrosis vs Sclerosis
Treatment approaches for fibrosis primarily involve antifibrotic medications such as pirfenidone and nintedanib, which aim to slow tissue scarring and preserve organ function. In contrast, sclerosis management often includes immunosuppressive therapies like corticosteroids and methotrexate to control immune system activity and reduce inflammation. Both conditions may benefit from supportive care, including physical therapy and symptom management tailored to the affected organs.
Prognosis and Long-Term Outcomes
Fibrosis involves excessive connective tissue buildup that can lead to organ dysfunction, whereas sclerosis refers to abnormal hardening or stiffening of tissue, often following fibrosis. Prognosis varies by organ affected, with fibrosis sometimes reversible in early stages, but sclerosis typically indicates more advanced and permanent tissue damage, resulting in poorer long-term outcomes. Early detection and targeted therapies improve survival rates and quality of life, especially in pulmonary and hepatic fibrosis compared to irreversible sclerosis.
Prevention Strategies and Lifestyle Modifications
Fibrosis and sclerosis involve abnormal tissue hardening, making early prevention strategies critical for maintaining organ function and overall health. Key lifestyle modifications include avoiding exposure to environmental toxins, maintaining a balanced diet rich in antioxidants, engaging in regular physical activity, and managing chronic conditions such as diabetes and hypertension to reduce inflammation and tissue damage. Monitoring at-risk populations through regular medical check-ups and adopting smoking cessation further support prevention efforts against the progression of fibrosis and sclerosis.
Recent Advances in Research and Therapeutic Innovations
Recent advances in fibrosis and sclerosis research highlight the identification of key molecular pathways such as TGF-b, PDGF, and the role of immune system dysregulation in tissue remodeling and chronic inflammation. Therapeutic innovations include the development of anti-fibrotic agents like pirfenidone and nintedanib, alongside emerging gene therapies and targeted biologics designed to attenuate extracellular matrix deposition and halt disease progression. Cutting-edge techniques such as single-cell RNA sequencing have enabled precise characterization of fibrotic cell populations, fostering personalized medicine approaches in managing these debilitating disorders.
Fibrosis Infographic
 libterm.com
libterm.com