Leukoplakia and erythroplakia are oral mucosal lesions that present with distinct white and red patches, respectively, often signaling potential precancerous conditions. Early detection and accurate diagnosis are vital for preventing progression to oral cancer and ensuring effective treatment. Explore the rest of this article to understand the signs, risks, and management options for these important oral health concerns.
Table of Comparison
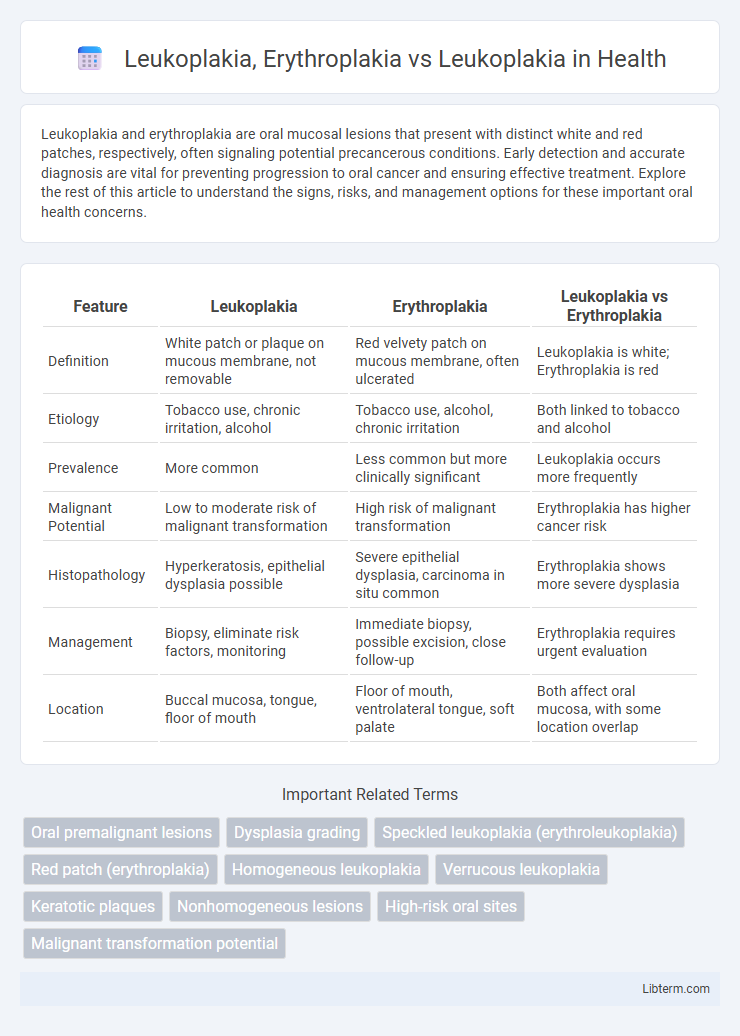
| Feature | Leukoplakia | Erythroplakia | Leukoplakia vs Erythroplakia |
|---|---|---|---|
| Definition | White patch or plaque on mucous membrane, not removable | Red velvety patch on mucous membrane, often ulcerated | Leukoplakia is white; Erythroplakia is red |
| Etiology | Tobacco use, chronic irritation, alcohol | Tobacco use, alcohol, chronic irritation | Both linked to tobacco and alcohol |
| Prevalence | More common | Less common but more clinically significant | Leukoplakia occurs more frequently |
| Malignant Potential | Low to moderate risk of malignant transformation | High risk of malignant transformation | Erythroplakia has higher cancer risk |
| Histopathology | Hyperkeratosis, epithelial dysplasia possible | Severe epithelial dysplasia, carcinoma in situ common | Erythroplakia shows more severe dysplasia |
| Management | Biopsy, eliminate risk factors, monitoring | Immediate biopsy, possible excision, close follow-up | Erythroplakia requires urgent evaluation |
| Location | Buccal mucosa, tongue, floor of mouth | Floor of mouth, ventrolateral tongue, soft palate | Both affect oral mucosa, with some location overlap |
Introduction to Leukoplakia and Erythroplakia
Leukoplakia and erythroplakia are distinct oral mucosal lesions primarily differentiated by their clinical appearance, with leukoplakia presenting as white patches and erythroplakia as red lesions. Leukoplakia is often associated with chronic irritation and has a variable potential for malignant transformation, frequently linked to tobacco use and alcohol consumption. Erythroplakia, although less common, carries a higher risk of malignancy and dysplasia due to its red, velvety, and well-demarcated presentation indicating significant epithelial atypia.
Definition and Clinical Features of Leukoplakia
Leukoplakia is defined as a white patch or plaque on the oral mucosa that cannot be rubbed off and cannot be characterized clinically or pathologically as any other disease. Clinically, leukoplakia presents as homogenous or non-homogenous white lesions, often asymptomatic, but may show areas of erythema or ulceration. Erythroplakia differs by appearing as a red, velvety patch, which carries a higher risk of dysplasia and malignant transformation compared to leukoplakia.
Definition and Clinical Features of Erythroplakia
Erythroplakia is defined as a red patch on the mucous membranes, predominantly in the oral cavity, that cannot be classified clinically or pathologically as any other condition. Clinically, erythroplakia presents as a well-demarcated, velvety red lesion often found on the floor of the mouth, tongue, or soft palate, and is associated with a higher risk of dysplasia or carcinoma compared to leukoplakia. Unlike leukoplakia, which appears as a white plaque with a lower malignant transformation rate, erythroplakia's intense erythema and fragile texture reflect severe epithelial abnormalities and a significantly elevated potential for malignancy.
Epidemiology and Prevalence of Oral Premalignant Lesions
Leukoplakia is the most common oral premalignant lesion with a global prevalence ranging from 1% to 5%, predominantly affecting middle-aged adults and males with tobacco use as a major risk factor. Erythroplakia, though less prevalent--occurring in less than 1% of the population--shows a higher malignant transformation rate, often affecting older adults with a history of alcohol and tobacco consumption. Epidemiological studies highlight leukoplakia's widespread occurrence across different regions, while erythroplakia is less frequently diagnosed but represents a more clinically significant risk for oral squamous cell carcinoma.
Etiology and Risk Factors: Leukoplakia vs Erythroplakia
Leukoplakia primarily develops due to chronic irritation from tobacco use, alcohol consumption, and mechanical trauma, with a higher prevalence in older adults and smokers. Erythroplakia, often linked to more severe epithelial dysplasia, shares similar risk factors but is more strongly associated with heavy tobacco and alcohol use, presenting a greater malignant potential. Both lesions arise from mucosal tissue subjected to carcinogenic exposure, yet erythroplakia exhibits a more aggressive pathogenesis with a significantly elevated risk for transformation into squamous cell carcinoma.
Pathological Differences Between Leukoplakia and Erythroplakia
Leukoplakia and erythroplakia are distinct oral mucosal lesions with different pathological characteristics; leukoplakia typically presents as a white patch due to hyperkeratosis and epithelial hyperplasia, while erythroplakia appears as a red patch caused by epithelial atrophy or dysplasia. Histologically, erythroplakia shows a higher prevalence of severe dysplasia, carcinoma in situ, or invasive carcinoma compared to leukoplakia, which often exhibits mild to moderate dysplasia. The increased risk of malignant transformation in erythroplakia makes its pathological evaluation critical for early diagnosis and management.
Malignant Transformation Potential: A Comparative Overview
Leukoplakia exhibits a malignant transformation rate ranging from 1% to 5%, whereas erythroplakia shows a significantly higher risk, with transformation rates reported between 20% and 50%. Histopathological evaluation reveals that erythroplakia often presents with severe dysplasia or carcinoma in situ, contributing to its greater malignancy potential compared to the predominantly hyperkeratotic changes seen in leukoplakia. Early detection and biopsy of erythroplakia lesions are critical due to their higher propensity for malignant progression relative to leukoplakia.
Diagnosis and Differential Diagnosis of Oral White and Red Lesions
Leukoplakia presents as white plaques that cannot be scraped off and require biopsy for diagnosis to exclude dysplasia or malignancy. Erythroplakia appears as red velvety patches, with a higher risk of severe dysplasia or carcinoma, necessitating prompt histopathological evaluation. Differential diagnosis involves distinguishing leukoplakia from other white lesions such as lichen planus, candidiasis, and frictional keratosis, while erythroplakia must be differentiated from inflammatory or vascular red lesions to ensure accurate treatment and monitoring.
Management and Treatment Strategies
Leukoplakia management primarily involves eliminating risk factors like tobacco and alcohol use, with regular monitoring and biopsy for suspicious lesions due to its potential premalignant nature. Erythroplakia requires more aggressive intervention, including prompt biopsy and often surgical excision, given its higher risk of dysplasia or carcinoma. Treatment strategies emphasize early detection, removal of etiologic factors, and close follow-up to prevent malignant transformation for both conditions.
Prognosis and Prevention: Key Takeaways
Leukoplakia presents a relatively lower risk of malignant transformation compared to erythroplakia, which carries a significantly higher potential for progressing to oral squamous cell carcinoma. Prevention strategies emphasize tobacco cessation, alcohol moderation, and regular oral screenings to detect early epithelial changes in both conditions. Early diagnosis through biopsy and histopathological evaluation is crucial for improving prognosis by guiding timely therapeutic interventions.
Leukoplakia, Erythroplakia Infographic
 libterm.com
libterm.com