Anemia occurs when your body lacks enough healthy red blood cells to carry adequate oxygen to tissues, causing fatigue and weakness. Common causes include iron deficiency, chronic diseases, and vitamin B12 shortages, each requiring specific treatments to restore normal blood levels. Discover more about anemia symptoms, diagnosis, and effective management in the rest of this article.
Table of Comparison
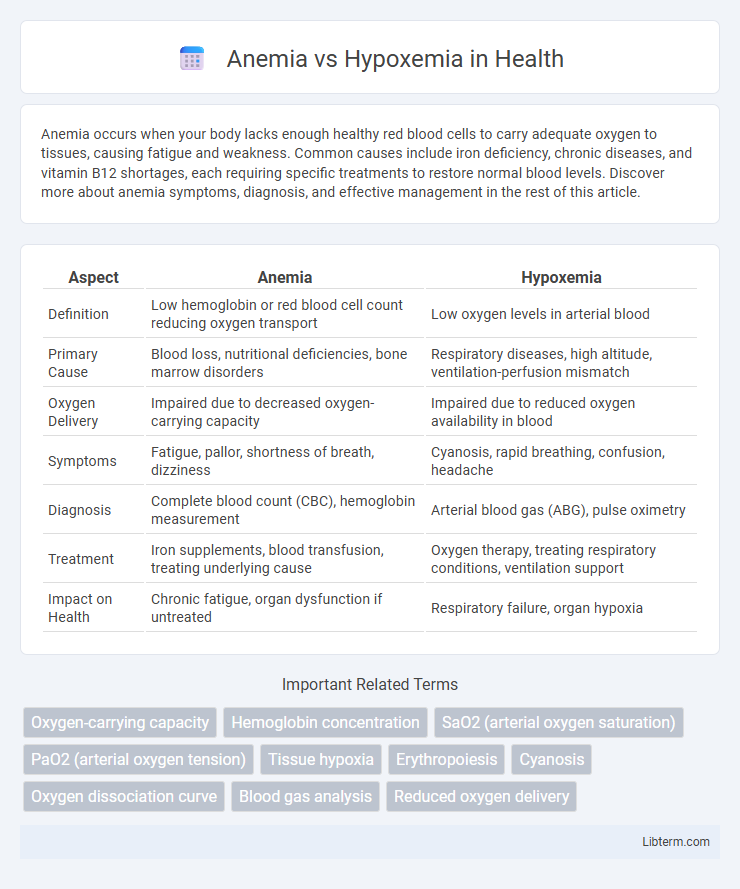
| Aspect | Anemia | Hypoxemia |
|---|---|---|
| Definition | Low hemoglobin or red blood cell count reducing oxygen transport | Low oxygen levels in arterial blood |
| Primary Cause | Blood loss, nutritional deficiencies, bone marrow disorders | Respiratory diseases, high altitude, ventilation-perfusion mismatch |
| Oxygen Delivery | Impaired due to decreased oxygen-carrying capacity | Impaired due to reduced oxygen availability in blood |
| Symptoms | Fatigue, pallor, shortness of breath, dizziness | Cyanosis, rapid breathing, confusion, headache |
| Diagnosis | Complete blood count (CBC), hemoglobin measurement | Arterial blood gas (ABG), pulse oximetry |
| Treatment | Iron supplements, blood transfusion, treating underlying cause | Oxygen therapy, treating respiratory conditions, ventilation support |
| Impact on Health | Chronic fatigue, organ dysfunction if untreated | Respiratory failure, organ hypoxia |
Understanding Anemia: Definition and Causes
Anemia is a condition characterized by a decreased number of red blood cells or insufficient hemoglobin, leading to reduced oxygen transport in the blood. Common causes include iron deficiency, vitamin B12 deficiency, chronic diseases, and bone marrow disorders. Unlike hypoxemia, which involves low oxygen levels in the blood, anemia primarily results from impaired oxygen-carrying capacity due to these underlying factors.
What is Hypoxemia? Key Features and Triggers
Hypoxemia is a medical condition characterized by low levels of oxygen in the blood, specifically a reduced partial pressure of oxygen (PaO2) below 80 mm Hg. Key features include cyanosis, shortness of breath, rapid heartbeat, and confusion resulting from insufficient oxygen delivery to tissues. Common triggers encompass respiratory diseases like chronic obstructive pulmonary disease (COPD), high altitudes, pneumonia, and impaired gas exchange in the lungs.
Pathophysiology: How Anemia and Hypoxemia Differ
Anemia involves a reduced concentration of hemoglobin or red blood cells, impairing the blood's oxygen-carrying capacity, whereas hypoxemia refers to low partial pressure of oxygen in arterial blood, indicating inadequate oxygen supply at the pulmonary or systemic level. In anemia, oxygen delivery is compromised despite normal oxygen saturation because the total hemoglobin is insufficient, while hypoxemia directly lowers arterial oxygen saturation, affecting oxygen availability to tissues. Pathophysiologically, anemia primarily affects oxygen content, and hypoxemia disrupts oxygen partial pressure gradients critical for diffusion.
Clinical Manifestations and Symptoms Comparison
Anemia primarily presents with fatigue, pallor, dizziness, and shortness of breath due to reduced oxygen-carrying capacity of hemoglobin, while hypoxemia manifests through cyanosis, tachypnea, confusion, and impaired cognition resulting from low arterial oxygen levels. Both conditions may cause dyspnea and tachycardia, but anemia commonly shows signs of tissue hypoxia without central nervous system compromise, whereas hypoxemia often leads to neurological symptoms due to cerebral oxygen deprivation. Pulse oximetry readings remain normal in anemia but are decreased in hypoxemia, aiding clinical differentiation.
Diagnostic Approaches: Anemia vs Hypoxemia
Anemia diagnosis primarily involves complete blood count (CBC) tests measuring hemoglobin levels, hematocrit, and red blood cell indices to identify decreased oxygen-carrying capacity. Hypoxemia diagnosis relies on arterial blood gas (ABG) analysis and pulse oximetry to assess the partial pressure of oxygen (PaO2) and oxygen saturation (SpO2), indicating reduced oxygen availability in the blood. Differentiating between anemia and hypoxemia is critical, as anemia reflects low hemoglobin content, whereas hypoxemia indicates impaired oxygen diffusion or transport despite normal hemoglobin.
Risk Factors and Populations at Higher Risk
Anemia primarily affects populations with nutritional deficiencies, chronic diseases, or genetic disorders such as sickle cell anemia and thalassemia, increasing their risk due to impaired red blood cell production or loss. Hypoxemia risk factors include chronic respiratory diseases like COPD, high altitudes, and conditions causing ventilation-perfusion mismatch, with higher susceptibility in elderly individuals and those with cardiovascular or pulmonary disorders. Both conditions show increased prevalence in premature infants and populations with limited access to healthcare or poor living conditions.
Laboratory Findings: Distinguishing Anemia from Hypoxemia
Laboratory findings in anemia typically reveal decreased hemoglobin concentration and hematocrit levels, indicating reduced oxygen-carrying capacity of the blood. In contrast, hypoxemia is characterized by low arterial oxygen partial pressure (PaO2) and oxygen saturation (SaO2) despite normal hemoglobin levels, reflecting impaired oxygenation rather than reduced red cell mass. Arterial blood gas analysis and complete blood count are essential diagnostic tools to differentiate anemia from hypoxemia based on their distinct laboratory profiles.
Treatment Strategies for Anemia and Hypoxemia
Treatment strategies for anemia focus on addressing the underlying cause, such as iron supplementation for iron-deficiency anemia, vitamin B12 or folate for megaloblastic anemia, and erythropoiesis-stimulating agents for chronic kidney disease-related anemia. Hypoxemia treatment aims to improve oxygenation through supplemental oxygen therapy, mechanical ventilation in severe cases, and addressing the root cause like lung diseases or cardiac conditions. Both require ongoing monitoring to adjust treatments based on patient response and oxygenation status.
Potential Complications and Prognosis
Anemia can lead to complications such as fatigue, heart failure, and impaired cognitive function due to reduced oxygen delivery to tissues, with prognosis improving through treatment of underlying causes and iron supplementation. Hypoxemia may cause acute respiratory distress, organ dysfunction, and increased risk of mortality if untreated, with prognosis depending on severity and timely intervention including oxygen therapy and addressing root causes. Both conditions compromise oxygen availability but differ in etiology, clinical management, and potential long-term outcomes.
Prevention, Management, and Patient Education
Preventing anemia involves a balanced diet rich in iron, vitamin B12, and folate, alongside managing chronic conditions that affect red blood cell production. Hypoxemia prevention focuses on avoiding respiratory irritants, ensuring proper management of lung diseases like COPD, and using supplemental oxygen when prescribed. Patient education emphasizes recognizing symptoms such as fatigue, pallor, or shortness of breath, adhering to prescribed treatments including iron supplements or oxygen therapy, and seeking timely medical follow-up to monitor blood oxygen levels and hemoglobin.
Anemia Infographic
 libterm.com
libterm.com